7.1. General principles of infection prevention and control.
-
Key infection control concepts and terms.
Infection: Is an invasion of the body tissue by pathogenic microorganism.
As a direct care staff person, an important part of your job is to protect yourself and the clients from infectious disease(s). Some clients have weakened immune systems and are more vulnerable to getting infections. An important part of maintaining a safe environment is to recognize signs of infection. This section will present several ways to control and limit the spread of germs that cause infections. Germs cause illness and disease. As a direct care staff person, you will come in contact with body fluids that may contain germs such as blood, mucous, vomit, tears, semen, vaginal secretions, saliva, urine, feces and sweat.
In order to prevent an infection from spreading, it is important to understand where germs live, how germs get to people and how germs enter people’s bodies. There are many “sources” of germs. These are places germs live before they infect. Sources include: under the fingernails, on the skin, on an unclean surface and in water and food. There are many germs on the kitchen counter and in the bathroom. Germs can be found almost everywhere, including: in the air, on surfaces, on your hands and in your nose. Germs can enter the body through any opening such as your nose, mouth or any opening such as cuts.
The Personal Care Worker must know the importance of cleanliness. You need to try to achieve ideal sanitary conditions. Cleanliness is an important part of controlling disease and keeping diseases from spreading. This unit will explain pathogens, the chain of infection, signs of infection, keeping surroundings clean, hand washing, and body substance isolation.
What are microorganisms?
Very small, living microorganisms are everywhere. Many are helpful to people. For instance, microorganisms in the human digestive tract break down foods and turn them into waste products when not used by the body. When microorganisms move out of their natural environment into a foreign one, they become pathogens. Pathogens are disease producing microorganisms. They destroy human tissue by using it as food and giving off a waste product called toxins. Toxins are absorbed into the body and poison it, causing an infection.
Signs of Infection
- Fever
- Restlessness
- Chills
- Abnormal discharge
- Swelling
- Lack of appetite
- Redness
- Pain
- Change in behavior.
- Confusion.
Report these signs to the care recipient’s Doctor or other responsible person.
-
Chain of infection, Infective process. Aseptic measures.
Chain of infection.
What is the chain of infection?
Whether or not an infection happens will depend on a number of things. It is best explained by looking at the ‘chain of infection’ which consists of six ‘links’ that have to be present for an infection to happen. The links are:
- Pathogen: Microorganism that causes disease.
- Reservoir: Where the pathogen lives and grows usually in warm, moist, dark places. Examples – cut or open area, bladder, and lungs.
- Portal of exit: How pathogen leaves one place or host. Examples – drainage & secretions, urine, stool, blood, breathing, sneezing, or coughing.
- Transmission: How pathogen is carried from portal of exit to portal of entry. Examples – hands, food, mouth, and clothing.
- Portal of Entry: How pathogen enters new place or host. Examples – cuts, mucous membranes (eyes, nose, mouth).
- Susceptible Host: Someone more likely to become infected. Elderly people are more susceptible due to aging changes.
You can stop the process by ‘breaking’ the chain and removing one of the links.
Some examples are:
- Reservoir: Keep cuts, etc. clean and uncovered. Keep surroundings clean.
- Portal of exit: Cover mouth and nose when coughing or sneezing. Cover open areas if draining.
- Transmission: Wash hands. Keep clothing clean by holding things away from you. Wear gloves, mask, and apron when needed.
By doing these things, you may stop an infection either to you or your care.
Infective process.
Modes and control of transmission
There are six common modes of transmission of infection. (See Table) If the mode of transmission is known, precautions can be put in place to prevent outbreaks. Precautions will vary according to the microorganism involved and the context of the case. For instance a case of influenza in a normal household setting does not require strict precautions, where as one in a long term care home might. In hospitals, the infection control team can be a source of advice on which precautions to use. Outside hospitals, the local public health authority can be consulted.
Modes of transmission of infections and corresponding ways of controlling spread. Note that the precautions to be taken vary with the microorganism and the context of the illness.
Contact Direct Direct physical contact (body surface to body surface) between infected individuals and susceptible hosts.Examples: Influenza virus; Infectious mononucleosis; chlamydia.Precautions: Hand hygiene; masks; condoms. Indirect An infectious agent deposited onto an object or surface (fomite) and survives long enough to transfer to another person who subsequently touches the object. Examples: RSV; Norwalk; rhinovirus; perhaps influenza.Precautions: Sterilizing instruments; disinfecting surfaces and toys in school. Droplet Via coughing or sneezing, or (in health care) during suctioning. Droplets are relatively large (>5 µm) and can be projected up to about one meter. Examples: Meningococcus; influenza (though there is some debate); respiratory viruses.Precautions: Masks; cover mouth; stand clear. Non-contact Airborne Transmission via aerosols (airborne particles <5µm) that contain organisms in droplet nuclei or in dusts. It can be spread via ventilation systems.Examples: TB; measles; chickenpox; smallpox (and maybe influenza: controversial, as more likely via droplets).Precautions: Masks; negative pressure rooms in hospitals. Vehicle A single contaminated source spreads the infection (or poison). This can be a common source or a point source.Examples) Point source: Food-borne outbreak from the infected batch of food; cases typically cluster around the site (such as a restaurant)b) Common source: The Listeriosis outbreak in Canada in 2008 was linked to a meat production facility in Ontario. It caused 20 cases across five provinces. Cases may be widely dispersed due to the transport and distribution of the vehicle. Precautions: Normal safety and disinfection standards. Deliberate contamination of Tylenol in 1982 led to the use of tamper-proof containers for medicines. Vector-borne Transmission by insect or animal vectors.Example: Mosquitoes malaria vector, ticks Lyme disease vector.Precautions: Protective barriers (window screens, bed nets); insect sprays; culling animals. - Immune response.
The human immune system has two levels of immunity: specific and non-specific immunity. Through non-specific immunity, also called innate immunity, the human body protects itself against foreign material that is perceived to be harmful. Microbes as small as viruses and bacteria can be attacked.
Aseptic measures.
Principles of ‘clean’/medical asepsis.
Medical asepsis (clean technique) all practices that reduce the number, growth, transfer and spread of pathogenic microorganisms. They include hand washing, bathing, cleaning environment, gloving, gowning, wearing masks, hair and shoe covers, disinfecting articles and use of antiseptics. You can prevent infection from spreading by providing clients with clean surroundings.
Principles of disinfection
Disinfection: Process of eliminating pathogenic organisms on an inanimate object with the exception of spores. Disinfectant: This is a chemical substance that kills most of the bacteria is used for disinfecting only an inanimate object e.g. (phenol, chlorine).Those bacteria that not killed are slowed in their growth. Reusable plastic bedpans, trays, and equipment are sanitized (washed in bacterial cleanser), dries, and stored in clean bags.
Antiseptic solution: Is a substance that is used on a person’s skin to inhibit the growth and activity of microorganisms, but not necessarily destroys them. Contamination: The process by which something is rendered unclean or unsterile
Concurrent disinfection; Practices that are done, on a day to day basis in the care of the patient, his lies, and his immediate environment to limit or control the spread of microorganisms.
Principles of sterility/Principles of surgical asepsis
Surgical asepsis (sterile technique); Practices that keep an area or objects free from all microorganisms nonpathogenic and pathogenic including spores and viruses. Sterilizing kills all bacteria. Unless bacteria are dead, an object is not sterile. A sterile object becomes contaminated when exposed to air or other objects. Diagnostic equipment and metal bedpans are most commonly sterilized by autoclaving (an intense heat process).
Cleanliness
One way to stop the spread of infection is by keeping the care recipient’s home clean. You can do this by following these guidelines:
- Hold linens and other supplies away from your body.
- Separate clean and dirty objects.
- Keep things off the floor. Anything that falls on the floor is considered dirty and must be cleaned appropriately before using it.
Cleaning and disinfecting – Keeping germs away:

Another critical method for preventing the spread of germs is the cleaning and disinfecting surfaces. Cleaning refers to washing with soap and water and disinfecting refers to the use of a cleaning product that kills bacteria and other germs. Disinfection is especially important in the kitchen and bathroom.
Some general steps are involved in the proper cleaning and disinfection of surfaces:
- Carefully follow directions and precautions on all cleaning products.
- Begin by cleaning the surface thoroughly with soap and water or another cleaner.
- After cleaning, if you need to use a disinfectant, apply it to the area and let it stand for a few minutes or longer following the directions on the product.
- Wipe the surface with a paper towel that can be thrown away or a cloth that will be washed immediately afterward.
- After cleaning or disinfecting, always wash hands, even if you wore gloves.
-
Hand washing.Using gloves.
Hand washing:
You use your hands constantly. The easiest and most important way of preventing the spread of infection is by hand washing. Washing your hands before and after caring for your care recipient will help to prevent the spread of microorganisms.
Good hand hygiene is important:
Hand washing seems like such an obvious thing to do, but numerous studies show that many people, including health care workers, often forget to wash their hands as thoroughly and frequently as they should.
When to wash hands:
- Before and after wearing gloves.
- At the start of the workday and several times throughout the day.
- When your hands are visibly soiled (dirty) or contaminated with blood or body fluids.
- Before having direct contact with the resident’s skin.
- After having direct contact with the resident’s skin, especially when the skin has wounds or is broken.
- After assisting with toileting or changing incontinence products from the resident.
- After the direct care worker uses the restroom.
- Before eating.
- Before preparing food.
- Before serving food.
- After wiping nose, sneezing or touching the face.
- Before and after each task.
- After smoking.
When washing your hands, some guidelines to follow are:
- If available, use a paper towel to turn water on and off.
- Rinse the bar of soap before and after using it.
- Avoid touching the sink and wastebasket with your hands.
- Do not lean against the sink.
- Rubbing, or friction, helps remove germs.
- Use enough soap to get a good lather.
- Rinse from above the wrists to fingertips.
- Make sure all equipment is available: Soap, Paper towels, Nail brush, if used, Wastebasket.
- Turn the faucet on with a paper towel if available, and adjust the water temperature.
- Throw the paper towel in the wastebasket.
- Wet your hands and wrist under running water.
- Rinse the bar of soap and work up a good lather.
- Wash hands and 2” above wrists. Rub vigorously. Make sure to get between fingers and nail beds.
- Use a nailbrush to clean under nails or rub fingertips against palm of hand to get soap under nails.
- Continue to wash your hands for 1-2 minutes.
- Rinse wrists and hands thoroughly.
- Dry your hands with paper towels if available and throw them in wastebasket.
- Turn off the faucet with a dry paper towel and throw in the wastebasket.
- Place 6-7 drops of the sanitizer into the palm of a clean, dry hand.
- Rub the hands together vigorously until the sanitizer evaporates completely.
- Proceed with care as usual.
- Wash hands with soap and water as soon as practical or after 10-15 applications.
Procedure: Hand washing
Instructions for Use of Sanitizer:
Using gloves to reduce risk of infection:
As a direct care staff person, you should use gloves when there is the possibility that you will have contact with blood, other potentially infectious material or items and surfaces contaminated with these materials. Wear gloves to carry materials that are soiled or contaminated, and carry the material so it does not touch any other surface, including your clothing. It is important to dispose of soiled material as soon as possible. For example, put soiled linens directly into the designated container and not on the floor. Do not leave soiled linens on the floor even for a short time, such as while you finish making the bed.
Putting on and taking off gloves:Before putting gloves on, remove all sharp jewelry and wash hands to remove germs. When putting the gloves on, begin by putting your fingers into the tips of the glove and then pull the entire glove over your clean hand. Remove gloves by pulling the glove inside out so that whatever has touched the glove remains untouched by your exposed skin.
Gloves are to be worn any time there is a risk of coming in contact with blood or body fluids. Gloves are available to all field employees upon request. They can be obtained from the receptionist or the supervisor.
Examples of events that require theuse of gloves:
- During procedures:
- Providing mouth care for patient;
- Touching, cleaning broken skin, or mucous membranes;
- Cleaning genital area;
- Handling utensils or supplies that are soiled with body fluids.
- Changing linens that are soiled with body fluids.
- Cleaning spills of body fluids or blood.
- Any time the employee has an opening in the skin on the hands (includes around nails).
- Wash and thoroughly dry hands before putting on gloves.
- Handle gloves carefully while putting them on.
- Never use gloves that have been torn or punctured.
- Change gloves between procedures and after contact with each patient.
- Wash hands between sets of gloves.
- Never clean and re-use disposable gloves.
- To remove gloves, peel them off one at a time, pulling them inside-out (with the contaminated side to the inside).
- Properly dispose of used gloves in the family’s trash receptacle.
Instructions for Proper Use of Gloves:
- Wash and thoroughly dry hands before putting ongloves.
- Handle gloves carefully while putting themon.
- Never usegloves thathave been tornor punctured.
- Change gloves between procedures and after contact with eachpatient.
- Wash hands between sets ofgloves.
- Nevercleanandre-use disposablegloves.
- Toremovegloves,peelthemoffoneatatime,pullingtheminside-out(withthecontaminated side to theinside).
- Properly dispose of used gloves in the family’s trashreceptacle.
-
Some infection control precautions in-home care setting.
Disposal of Sharps:
Client-generated sharps, i.e. insulin syringes, should be placed in a puncture-resistant container in the home, perhaps a coffee can or liquid detergent bottle, etc. When full, the container should be firmly sealed with duct tape or other household tape and placed in the patient’s trash receptacle.
Disposal of Patient Wastes:
- Wear gloves.
- Flush feces, urine, and emesis down the toilet. Avoid splashing.
- Dispose of soiled items, dressings, incontinence supplies, gloves, and catheters by wrapping materials in plastic bag, brown paper bag, or newspaper, then placing in a plastic bag with patient’s other trash. Double-bag immediately and discard with regular garbage
Bed Linen.
Use precautions when handling bed linens. Solid linen can transfer germs. Follow these guidelines:
- Wash your hands before handling linen.
- Avoid touching linen with your clothing.
- Bring into the room only the linen to be used at that time.
- Keep clean and dirty linen separates.
- Wear gloves to handle linen that is soiled with blood or body fluids.
- Always roll soiled linen away from you, and avoid shaking or fluffing the linen.
- Keep all linen (clean and soiled) off the floor.
- Always wash your hands after handling soiled linen.
Jewelry:
Another thing personal care staff persons can do to reduce the spread of germs is to limit their wearing of jewelry. This is because the tiny surfaces and crevices on rings and other jewelry can serve as a breeding ground for germs. If you choose to wear a ring, keep it simple. Since fingernails can serve as a breeding ground for germs, keep your nails short and clean.
-
Centers for Disease Control and Prevention (CDC) guidelines.
Centers for Disease Control and Prevention (CDC) guidelines: www.cdc.gov
Precautions establish safe practices to protect healthcare workers. Universal Precautions were established in 1988 to prevent the spread of deadly blood-borne pathogens. Standard Precautions Developed in 1996, promote the use of personal protective equipment (e.g. gloves, gowns, masks, and eyewear) for contact with all body fluids (except sweat). Infected people often have no symptoms and may not know they are infected. Therefore, consider yourself at risk from everyone. Follow infection control practices and procedures at the facility where you work. Precautions reduce the risk of spreading germs from person to person.
Provide quality care for all clients, and use precautions with each person, all used needles, and all body fluids.
Assume all blood, body fluids, and needles are potentially infectious. Gloves must be worn at all times when handling these materials. Always wash your hands before and after wearing gloves.
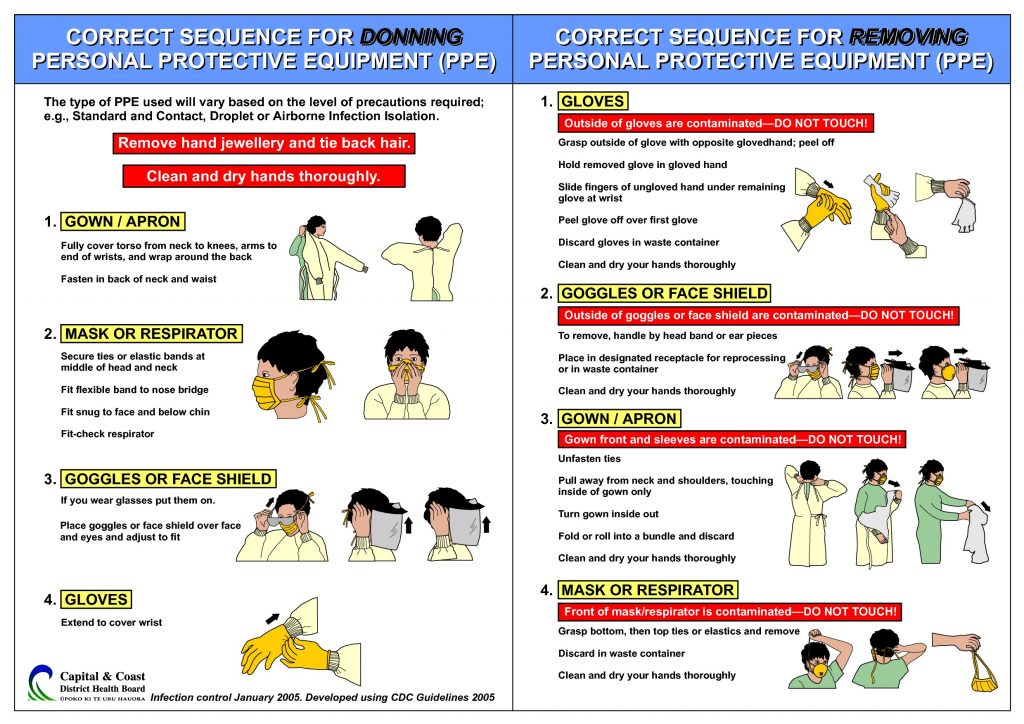
Personal Protective Equipment
Gloves, gowns, aprons, masks, and protective eyewear are necessary whenever you might be exposed to blood or body fluids, non-intact skin, and mucous membranes (mouth, nose, eyes, genital area). Personal protective equipment (PPE) is a barrier between you and possible sources of infection.
Gloves reduce the risk of spreading infection. Always wear disposable gloves whenever you have contact with any of the following:
- bleeding or open wounds (skin rashes, broken skin, pressure ulcers);
- other body fluids, including blood;
- Soiled linen.
Follow these guidelines for using gloves:
- Check for cracks, punctures, tears, or discoloration, and discard if damaged.
- Check for proper fit; avoid wrinkles.
- Wash your hands before putting on gloves.
- Pull gloves over gown cuffs if a gown 1sworn.
Change gloves whenever they become soiled to avoid spreading infection from one part of the body to another. Dispose of gloves after each resident contact.
To remove gloves, use one gloved hand lo grasp the other glove near the wrist and peel off the glove, pulling it inside-out. Hold it in the gloved hand. Slide fingers from the bare hand under the wrist of the other glove, peel off, creating a bag for both gloves. Dispose in the designated bin for infectious waste, and wash your hands.
Face masks may be required to protect residents, workers, and visitors from infection caused by air borne pathogens or exposure to blood and body fluids. Wash your hands before touching the mask. Pick up the mask by the straps, and avoid touching the part that covers your nose and mouth.
Masks should be changed frequently and anytime they become damp or wet. Dispose of used masks immediately in the appropriate waste container, and wash your hands.
Gowns are effective barriers to infection whenever you have direct contact with infectious material or body fluids. Roll your sleeves above your elbows, and wash your hands before putting on a gown.
Before removing the gown, remove and dispose of the gloves. Pull the gown away from neck and shoulders. Holding the gown away from you, turn it inward, keeping it inside out. Place the gown in the appropriate container, and wash your hands.
Isolation
Patients/clients with highly transmissible diseases are sometimes isolated (set apart) to protect others from infection. In addition to using Standard Precautions, you may be instructed to follow transmission-based precautions–contact, droplet, and airborne precautions – that vary according to the specific disease and how the pathogens are transmitted. Sometimes isolation is ordered for clients who cannot fight infection due to age, illness, or medications.
Doctors order isolation precautions. Instructions are generally posted on the door of isolation rooms. The instructions may direct all visitors to report to the nurses’ station before entering the room. Or, the signs may specify that personal protective equipment – gowns, masks, and gloves – is required each time anyone enters the room.
PERSONAL CARE WORKERS WILL NOT ORDINARILY BE ASSIGNED TO CLIENTS WHOSE CARE REQUIRES THE USE OF MASKS, GOGGLES, OR OTHER PERSONAL PROTECTIVE EQUIPMENT.
-
Standard Precautions. Personal Protective Equipment.
Standard precautions.
Standard precautions are the minimum infection prevention practices that should be used in the care of all patients/clients all of the time. These practices are designed to both protect the healthcare worker and to prevent the healthcare worker from spreading infections among patients.
Standard precautions include:
- Hand hygiene,
- Use of personal protective equipment (e.g., gloves, gowns, masks),
- Safe injection practices,
- Safe handling of potentially contaminated equipment or surfaces in the patient environment, and
- Respiratory hygiene/cough etiquette.
Isolation precautions.
Isolation precautions are used to help stop the spread of germs from one person to another. These precautions protect patients, families, visitors, and healthcare workers from the spread of germs.

Generally, when patients are placed on isolation precautions, there will be a sign at the door of their hospital rooms to remind visitors and healthcare workers which isolation precautions are needed. All healthcare workers and visitors need to follow these guidelines. Healthcare workers should not eat or drink in isolation rooms and should always clean their hands before entering the room and upon exiting the room.
Transmission based.
Contact Isolation Precautions—used for infections, diseases, or germs that are spread by touching the patient or items in the room (examples: MRSA, VRE, diarrheal illnesses, open wounds, RSV).
Healthcare workers should:
- Wear a gown and gloves while in the patient’s room.
- Remove the gown and gloves before leaving the room.
- Clean hands (hand washing or use hand sanitizer) when entering and leaving the room.
- Visitors must check with the nurse before taking anything into or out of the room.
Droplet/airborne precautions.
Droplet Isolation Precautions—used for diseases or germs that are spread in tiny droplets caused by coughing and sneezing (examples: pneumonia, influenza, whooping cough, bacterial meningitis).
Healthcare workers should:
- Wear a surgical mask while in the room. Mask must be discarded in trash after leaving the room.
- Clean hands (hand washing or use hand sanitizer) when they enter the room and when they leave the room.
Airborne Isolation Precautions—used for diseases or very small germs that are spread through the air from one person to another (examples: Tuberculosis, measles, chickenpox).
Healthcare workers should:
- Ensure patient is placed in an appropriate negative air pressure room (a room where the air is gently sucked outside the building) with the door shut.
- Wear a fit-tested NIOSH-approved N-95 or higher level respirator while in the room. Mask must be discarded in trash after leaving the room.
- Clean hands (hand washing or use hand sanitizer) when they enter the room and when they leave the room.
- Ensure the patient wears a surgical mask when leaving the room.
- Instruct visitors to wear a mask while in the room.
Respiratory hygiene/cough etiquette.
Respiratory hygiene and cough etiquette are infection prevention measures to decrease the transmission of respiratory illness such as influenza or cold viruses in healthcare facilities where patients, clients, employees, and visitors may not be immediately recognized as having a respiratory infection. These measures are part of the standard precautions that should be taken to prevent the spread of disease. Important elements include:
- Education of patients, families, visitors, clients and care providers about how respiratory infections are transmitted and how respiratory illness can be prevented. Ask family members, visitors, and care providers to stay home if they are sick.
- Use of posted signs with instructions and pictures about how to cover your cough and wash your hands.
- Availability and use of tissues when coughing and sneezing, and reminders to dispose of used tissues properly.
- Use of a mask for a person who is coughing.
- Physical separation of the person with a respiratory infection from others.
- Stressing hand hygiene after contact with respiratory secretions. This applies to the patient, family members, visitors, employees, and care providers.
- Nosocomial infection (Hospital acquired infection): It is an infection acquired from health care settings. It may be exogenous infection when part of the client’s flora become altered and an over growth results.
Nosocomial infections.
- Nosocomial infection (Hospital acquired infection): It is an infection acquired from health care settings. It may be exogenous infection when part of the client’s flora become altered and an over growth results.
Vaccination can prevent Hepatitis B infection.
- Hepatitis B Virus (HBV) is a viral infection of the liver. The disease causes fatigue, mild fever, muscle and joint pain, nausea, vomiting, and loss of appetite. There is no known cure for HBV at this time. HBV usually spreads through contact with infected blood, blood products, body fluids, or anywhere blood is present.
-
Preventing HIV/AIDS.
Always use precautions with all body fluids, especially blood.
AIDS (Acquired Immune Deficiency Syndrome) is a life-threatening condition caused by a virus known as HIV (Human Immunodeficiency Virus). The virus cripples the immune system, the body’s natural defense against disease. By destroying cells, HIV interferes with the ability to fight off viruses, bacteria, and fungi. The term AIDS refers to the later stages of HIV infection.
There is no cure and no vaccine at this time for HNIAIDS. The best defense is preventive education. It is important to understand how the disease spreads and how to protect yourself and others.
You will not get AIDS from casual contact. The disease is transmitted when contaminated (infected) fluid enters the bloodstream. Of these fluids, blood is the most common concern for healthcare workers.
Following are ways the virus enters the body: intimate sexual contact
- Transfusions with infected blood.
- Puncture wounds from infected needles or broken glass.
- Cuts or open sores.
- Mucous membranes (nose, mouth, eyes).
- Use of infected hypodermic needles.
- Infected mothers to their unborn babies
When people are infected with HIV, they are carriers for life. People may not know they are infected. Some carriers never show symptoms, but they can still transmit HIV to others.
Symptoms vary from person to person. In the early stages, people with HIV usually look and feel healthy. Early symptoms are often similar to common illnesses-coughing, fever, swollen glands, diarrhea. The symptoms go away, but the HIV remains in the body. Advanced symptoms may develop five to fourteen years later.
AIDS victims are susceptible to diseases the body would normally resist. As the disease progresses, the immune system is unable to fight infection. Treatment can increase the length of survival, but there is no cure.
Always use precautions to protect yourself and others from infection. Treat all blood and body fluids as contaminated. Wear gloves whenever you have contact with body fluids or soiled articles. Wash your hands with soap and water after any contact with blood, even if gloves are worn. Use the same precautions with vaginal secretions and semen.
Pour all liquid waste containing blood down the toilet. Avoid splashing on yourself. Put the toilet lid down, and flush. Also flush tissues and other flush able items with blood or body fluids on them. Use a disposal bag for paper towels, wound dressings, sanitary pads, and other solid waste. Close the bag securely. Follow disposal regulations for the facility where you work.
Summary
Protect yourself, clients, co-workers, and visitors from infection by using precautions. The best defense is understanding how infection spreads and using preventive measures. Thorough hand washing is the single most important preventive measure for infection control. Other important measures include clean surroundings, personal protective equipment, and isolation precautions. Always protect clients from infection, provide quality care, and treat all body fluids and needles as potentially infectious.
All basic supplies and equipment for the care of the isolated client should be stored in the room. Gather any additional equipment before you put on isolation gear to enter the room.
It is not uncommon for isolated clients to be lonely and depressed. The PCW can help ease depression in a variety of ways. Following are examples.
- Check on the person often, and answer the call signal promptly.
- Spend time with the client.
- Provide access to television, radio, magazines, puzzles and other amusements.
- Tell the client when you will be back, and be prompt; let the client know if you are delayed.
- Be cautious of what you say outside the room; the client may hear you.
- Help the client, family, and visitors be comfortable and confident with the isolation procedures.
Other Precautions
Use extreme caution with needles and infectious waste. Be aware of how infection is spread, and use personal protective equipment to protect yourself and others from infection.
Following are additional precautions and safety measures.
- Handle all needles very carefully, and dispose of them in designated biohazard containers.
- Be aware that gloves will not protect you from being stuck by a needle. If you stick yourself with a used needle, wash the punctured area immediately with hot, soapy water. Then tell your supervisor.
- Be very careful whenever you handle infectious waste. Follow the facility’s guidelines for handling waste.
- Report all broken skin contact, mucous membrane contact, and puncture wounds.
- Change gloves each time you go from one client to another.
- Wear a mask, gown, gloves, and protective eyewear for any procedures that could involve blood or body fluid splashing.
- If you are pregnant and working in a high-risk area, get medical counseling.
-
Occupational Safety and Health Administration (OSHA) Guidelines.
Occupational Safety and Health Administration (OSHA) Guidelines: www.osha.gov
Blood borne pathogens are infectious microorganisms present in blood that can cause disease in humans. These pathogens include, but are not limited to, hepatitis B virus (HBV), hepatitis C virus (HCV), and human immunodeficiency virus (HIV), the virus that causes AIDS. Workers exposed to blood borne pathogens are at risk for serious or life-threatening illnesses.
Body Substance Isolation Body Substance Isolation (BSI) is the practice of how to handle and dispose of body fluids in a safe manner to prevent the spread of infection. It focuses on isolating all moist and potentially infectious body substances, such as blood, feces, urine, sputum, and wound drainage, from all persons. BSI includes thorough hand washing, the use of gloves and plastic aprons, and proper disposal of both body fluids and the items used. It means using gloves when handling anything warm, wet, and not yours. Plastic aprons should be worn when splashing or soiling is likely. Waste such as soiled gloves, bloody bandages, or soiled briefs and pads should be put in a plastic bag and closed. That bag can then be put in with the regular garbage and placed in the trashcan. This way the waste is in two bags. Blood spills need to be cleaned up in a special way. You can use a disinfectant made from one part bleach and ten parts water. You should wear gloves and use paper towels to clean the area. The waste (towels and gloves) should go into a plastic bag and closed. Again, that bag should be put in the regular garbage and placed in a trashcan. Following these recommendations will help to avoid the spread of infection and to keep you and your care recipient healthy.
Exposure control plan.
In general, the standard requires employers to:
- Establish an exposure control plan. This is a written plan to eliminate or minimize occupational exposures. The employer must prepare an exposure determination that contains a list of job classifications in which all workers have occupational exposure and a list of job classifications in which some workers have occupational exposure, along with a list of the tasks and procedures performed by those workers that result in their exposure.
- Employers must update the plan annually to reflect changes in tasks, procedures, and positions that affect occupational exposure, and also technological changes that eliminate or reduce occupational exposure. In addition, employers must annually document in the plan that they have considered and begun using appropriate, commercially-available effective safer medical devices designed to eliminate or minimize occupational exposure. Employers must also document that they have solicited input from frontline workers in identifying, evaluating, and selecting effective engineering and work practice controls.
- Implement the use of universal precautions (treating all human blood and OPIM as if known to be infectious for blood borne pathogens).
- Identify and use engineering controls. These are devices that isolate or remove the blood borne pathogens hazard from the workplace. They include sharps disposal containers, self-sheathing needles, and safer medical devices, such as sharps with engineered sharps-injury protection and needleless systems.
- Identify and ensure the use of work practice controls. These are practices that reduce the possibility of exposure by changing the way a task is performed, such as appropriate practices for handling and disposing of contaminated sharps, handling specimens, handling laundry, and cleaning contaminated surfaces and items.
- Provide personal protective equipment (PPE), such as gloves, gowns, eye protection, and masks. Employers must clean, repair, and replace this equipment as needed. Provision, maintenance, repair and replacement are at no cost to the worker.
- Make available hepatitis B vaccinations to all workers with occupational exposure. This vaccination must be offered after the worker has received the required blood borne pathogens training and within 10 days of initial assignment to a job with occupational exposure.
- Make available post-exposure evaluation and follow-up to any occupationally exposed worker who experiences an exposure incident. An exposure incident is a specific eye, mouth, other mucous membrane, non-intact skin, or parenteral contact with blood or OPIM. This evaluation and follow-up must be at no cost to the worker and includes documenting the route(s) of exposure and the circumstance under which the exposure incident occurred; identifying and testing the source individual for HBV and HIV infectivity, if the source individual consents or the law does not require consent; collecting and testing the exposed worker’s blood, if the worker consents; offering post exposure prophylaxis; offering counseling; and evaluating reported illnesses. The healthcare professional will provide a limited written opinion to the employer and all diagnoses must remain confidential.
- Use labels and signs to communicate hazards. Warning labels must be affixed to containers of regulated waste; containers of contaminated reusable sharps; refrigerators and freezers containing blood or OPIM; other containers used to store, transport, or ship blood or OPIM; contaminated equipment that is being shipped or serviced; and bags or containers of contaminated laundry, except as provided in the standard. Facilities may use red bags or red containers instead of labels. In HIV and HBV research laboratories and production facilities, signs must be posted at all access doors when OPIM or infected animals are present in the work area or containment module.
- Provide information and training to workers. Employers must ensure that their workers receive regular training that covers all elements of the standard including, but not limited to: information on blood borne pathogens and diseases, methods used to control occupational exposure, hepatitis B vaccine, and medical evaluation and post-exposure follow-up procedures. Employers must offer this training on initial assignment, at least annually thereafter, and when new or modified tasks or procedures affect a worker’s occupational exposure. Also, HIV and HBV laboratory and production facility workers must receive specialized initial training, in addition to the training provided to all workers with occupational exposure. Workers must have the opportunity to ask the trainer questions. Also, training must be presented at an educational level and in a language that workers understand.
- Maintain worker medical and training records. The employer also must maintain a sharps injury log, unless it is exempt under Part 1904 — Recording and Reporting Occupational Injuries and Illnesses, in Title 29 of the Code of Federal Regulations.
Occupational Safety and Health Administration www.osha.gov 1-800-321-6742
Be sure your facility’s Exposure Control Plan meets OSHA’s criteria.
According to the OSHA Blood borne Pathogens Standard, an Exposure Control Plan must meet certain criteria:
- It must be written specifically for each facility;
- It must be reviewed and updated at least yearly (to reflect changes such as new worker;
- Positions or technology used to reduce exposures to blood or body fluids);
- It must be readily available to all workers.
Exposure incidents and reports.
OSHA’s Blood borne Pathogens standard (29 CFR 1910.1030) requires employers to make immediate confidential medical evaluation and follow-up available for workers who have an exposure incident, such as a needle stick. An exposure incident is specific eye, mouth, other mucous membrane, non-intact skin, or parenteral contact with blood or other potentially infectious materials (OPIM), as defined in the standard that results from the performance of a worker’s duties.
Reporting an Exposure Incident
Exposure incidents should be reported immediately to the employer since they can lead to infection with hepatitis B virus (HBV), hepatitis C virus (HCV), human immunodeficiency virus (HIV), or other blood borne pathogens. When a worker reports an exposure incident right away, the report permits the employer to arrange for immediate medical evaluation of the worker. Early reporting is crucial for beginning immediate intervention to address possible infection of the worker and can also help the worker avoid spreading blood borne infections to others. Furthermore, the employer is required to perform a timely evaluation of the circumstances surrounding the exposure incident to find ways of preventing such a situation from occurring again. Reporting is also important because part of the follow-up includes identifying the source individual, unless the employer can establish that identifications infeasible or prohibited by state or local law, and determining the source’s HBV and HI infectivity status. If the status of the source individual is not already known, the employer is required to test the source’s blood as soon as feasible, provided the source individual consents. If the individual does not consent, the employer must establish that legally required consent cannot be obtained. If state or local law allows testing without the source individual’s consent, the employer must test the individual’s blood, if it is available. The results of these tests must be made available to the exposed worker and the worker must be informed of the laws and regulations about disclosing the source’s identity and infectious status.
Medical Evaluation and Follow-up
When a worker experiences an exposure incident, the employer must make immediate confidential medical evaluation and follow-up available to the worker. This evaluation and follow-up must be: made available at no cost to the worker and at reasonable time and place; performed by or under the supervision of a licensed physician or other licensed healthcare professional; and provided according to the recommendations of the U.S. Public Health Service (USPHS) current at the time the procedures take place. In addition, laboratory tests must be conducted by an accredited laboratory and also must be at no cost to the worker. Worker who participates in post-exposure evaluation and follow-up may consent to have his or her blood drawn for determination of a baseline infection status, but has the option to withhold consent for HIV testing at that time. In this instance, the employer must ensure that the worker’s blood sample is preserved for at least 90 days in case the worker changes his or her mind about HIV testing. Post-exposure prophylaxis for HIV, HBV, and HCV, when medically indicated, must be offered to the exposed worker according to the current recommendations of the U.S. Public Health Service. The post-exposure follow-up must include counseling the worker about the possible implications of the exposure and his or her infection status, including the results and interpretation of all tests and how to protect personal contacts. The follow-up must also include evaluation of reported illnesses that may be related to the exposure.
Written Opinion
The employer must obtain and provide the worker with a copy of the evaluating healthcare. Professional’s written opinion within 15 days of completion of the evaluation. According to OSHA’s standard, the written opinion should only include: whether hepatitis B vaccination was recommended for the exposed worker; whether or not the worker received the vaccination, and that the healthcare provider informed the worker of the results of the evaluation and any medical conditions resulting from exposure to blood or OPIM which require further evaluation or treatment. Any findings other than these are not to be included in the written report.
Additional Information
For more information, go to OSHA’s Blood borne Pathogens and Needle stick Prevention Safety and Health Topics web page at: https://www.osha.gov/SLTC/bloodbornepathogens/index.html
Occupational Safety And Health Administration
www.osha.gov 1-800-321-6742