7. Medication errors
-
7.1. Medication errors
 Knowing the following before administering medications will help prevent medication errors:
Knowing the following before administering medications will help prevent medication errors:- Name (generic and trade);
- Purpose;
- Effect;
- Length of time to take effect;
- Side effects;
- Adverse effects;
- Interactions;
- Special instructions;
- Where to get help;
- Six rights of medication.
A medication error occurs when
1. One of the “six client rights” has been violated.
- Administering wrong medication
- Administering wrong dose of medication
- Administering medication at the wrong time Medications may be administered per agency policy prior or per agency policy past the time ordered, and still be considered to be on time.
- Administering the medication in the wrong route (i.e. dermatological ointment administered to eye).
- Administering medication to wrong individual.
- Failing to document medication was given or inaccurate documentation of medicine give.
2. Staff
- Failure to comply with physician orders, failure to administer only upon current orders or occurs when the administration of a medication is not as prescribed by the doctor or prescribing practitioner; when a medication is administered in any way other than how it was prescribed. (Medication administered contrary to a physician’s order that either causes or has the potential to cause harm to the recipient.).
- Does not follow manufacturer’s directions.
- Does not follow accepted standards for medication administration.
- Failure to accurately transcribe a MAR.
- Improper documentation on MAR.
- Failure to accurately label a MRB.
- Improper medication storage.
- Running out of medications.
- Crushing a medication that shouldn’t be crushed
Medication error procedures:
- Immediately document details of the error on the MAR. Example: Giving the wrong client the wrong medication: Initial the appropriate date box, circle the initials, document the exact reason on the reverse side (or other designated area) of the MAR, and contact the appropriate person according to facility policy.
- Immediately notify the supervisor and physician. Follow agency policy to notify appropriate professionals
- Know and follow your facility’s policy for medication errors. Complete a medication error report in accordance with regulations and agency policies. The non-licensed personnel has the responsibility to ALWAYS follow agency policy and procedure to report if they have any reason to believe they have made a medication error. This should be reported as soon as possible.
- It is in regulation that medication errors are required to be reported to the licensing agency (Medicaid or CDPHE) within one business day.
- QMAP has been counseled about similar neglect in the previous 12 months and had been counseled and/or re-educated. Or the QMAP intentionally failed to follow the standard of practice or the facility’s policy with significant potential for harm or harm.
Considerations in determining if a medication error occurred:
- Medication error resulting in medical treatment.
- Medication error resulting in harm or the potential to cause harm.
Medication errors may result in adverse reactions to the individual. These reactions could range from a rash to death.
-
7.2. Storage requirements for medications kept in labeled containers or medication reminder boxes.
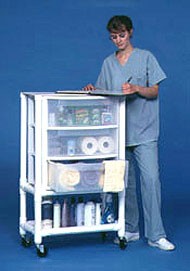 Storage of Medications
Storage of Medications- Medication storage areas, i.e., medication cart and medication room, need to be orderly so medication may be found easily.
- Store medications in a locked area, unless medications are under the direct supervision of staff; direct supervision means the cart is in sight and the staff person can get to the cart quickly, if necessary.
- Lock medication room/cart/cabinet when not in use. Unless the medication storage area is under the direct supervision of staff lock the medication, area including carts.
- Store external and internal medications in separate designated areas.
- Store refrigerated medications in the medication refrigerator or locked container if stored in refrigerator accessible to other staff.
- Store medications requiring refrigeration at 36 degrees F to 46 degrees F (2 degrees C to 8 degrees C)
Prescription and non-prescription medications:
- Store “in a manner that ensures the safety” of clients;
- Clients shall not have access to medication which is kept in a locked central location;
- Locked central location recommended, however, alternatives are acceptable if:
- Closed and locked drawer in client’s room in assisted living residence;
- Closed backpack, purse or on the person of client of sound mind in adult day facility;
- Closed wheelchair bag of non-ambulatory person in adult day facility;
- Closed and locked file drawer in administrative area inaccessible to clients.
Medications requiring refrigeration
I. Shall be stored separately in locked containers or compartmentalized packages, containers, or shelves for each client in order to prevent intermingling of medication.
II. If there is a designated medication refrigerator and the refrigerator is in a locked room, then the medications do not need to be stored in locked containers
Controlled substances:
 A. Must be doubled-locked, counted and signed for using a second person for verification. Example: Locked portable medication box stored inside locked cabinet. QMAP counts number of pills, second QMAP or qualified manager watches and agrees the count is correct. Shift to shift count for accuracy should include the date, time, quantity remaining, and signatures of both staff.
A. Must be doubled-locked, counted and signed for using a second person for verification. Example: Locked portable medication box stored inside locked cabinet. QMAP counts number of pills, second QMAP or qualified manager watches and agrees the count is correct. Shift to shift count for accuracy should include the date, time, quantity remaining, and signatures of both staff.
B. Any discrepancy, report immediately to supervisor for suspicion/investigation of drug diversion.
C. What if a second person is not available? QMAP counts number of pills and signs. Next QMAP on duty shall verify the count and sign the narcotic count sheet prior to administering; discrepancy immediately reported to supervisor.
D. Count how often?- At the end of each shift;
- Any time medication is given to a third party to take outside facility; count leaving and count upon returning.
Medication should not be stored with other items, must never be in areas with:
- Disinfectants;
- Insecticides;
- Bleaches;
- Household cleaners;
- Poisons