4. Documenting Medications (MAR).
-
4.1. Medication Administration Record (MAR)
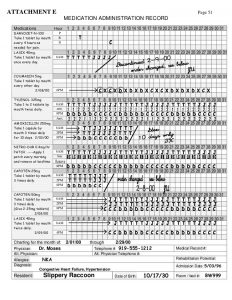
Form Commonly Used to Transcribe Medication Orders – Medication Administration Record (MAR)
- Each resident has a medication administration record (MAR);
- Form onto which medication and treatment orders are transferred;
- Record of all medications and treatments to be administered;
- Record of staff who administered medications;
- Record of medication not administered and the reason;
- Record of staff who administered medications.
-
4.2. The rules for documenting medications

- The Medication Administration Record (MAR) is a legal document. Documentation must be accurate.
- The document immediately after giving or monitoring medications, not before.
- Document each administration or monitoring at the time
- Only document medications that you administer or monitor.
- Initial medications are given or monitored in the box for the corresponding date and time.
- Always use black ink, never use a pencil
- Never use white-out or attempt to erase an error
- Not documented, not administered/monitored
- No blanks on the MAR
-
4.3. Transcription of Orders onto MAR
How to Read & Transcribe Prescription Orders
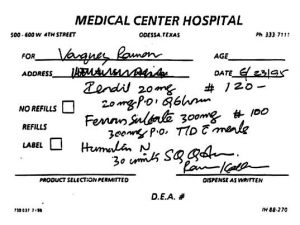
Reading Prescriptions

• Medication prescriptions are written by Licensed Practitioners.
• The Practitioner’s handwriting may be difficult to read however, it is the responsibility of the Pharmacist to ensure clarity of the prescription order.
Transcribing Medication Orders:
- Once a medication has been ordered and dispensed by the Pharmacy, it will be the responsibility of the employee to ensure accurate and timely transcription of the medication onto the correct Medication Administration Record, according to agency protocol.
- Writing legibly is very important when transcribing medications. This can prevent medication errors, and ensure client safety in medication administration.
- Only agency approved abbreviations should be used when transcribing medications
- All orders should be transcribed exactly as written. If the order is written with an unapproved abbreviation, a prescribing practitioner must be called for clarification.
- It is important to compare medications transcribed to medications on hand when preparing monthly Medication Administration Records.
Transcribe means to write down or to copy
In medication administration, it means to copy medication or treatment orders onto the MAR
- Orders are copied onto the MAR when the order is obtained or written
– Initial or sign and date orders written on the MAR
– Transcribe using proper abbreviations or written out completely; include all components of a medication order
– Count number of dosages to be administered instead of the number of days when calculating stop dates for medication orders that have been prescribed for a specific time period, such as antibiotics
– Do not schedule PRN orders for administration at specific times; they are administered when resident “needs” the medication for a certain circumstance
- A discontinue order must be obtained for an order to be discontinued unless the prescribing practitioner has specified the number of days or dosages to be administered or indicates that the dosage is to be changed.
-
4.4. Documenting on the Medication Administration Record (MAR)
- Discontinued meds: Write the date and DC large then draw a line through the rest of the dates and indicate discontinued; use a transparent yellow marker to highlight the name of the discontinued medication.
- New meds: transcribe new medications at the bottom of the list; draw a line through dated boxes up to the start date.
- To create a new MAR, copy from the physician orders. NEVER copy from the old MAR sheet.
- Each medication must be documented at the time of administration. For example, if eight medications are administered the QMAP must initial the MAR eight times indicating that each medication has been administered, refused or unavailable.
- New order: transcribe new medications on the MAR. Good practice is to keep routine and prn medications on the MAR.
- Follow your facility policies and procedures re: notification of new medications.
What to do if:
- You make a charting documentation error: Draw a single line through the mistaken entry and initial and date. Explain on the back of the MAR.
- Medication cannot be administered because it is not available or is refused: Circle the date box with your initials, document the exact reason on the reverse side (or other designated area) of the MAR, and contact the appropriate person according to facility policy.
- Give the client the wrong dose of medications: report to supervisor and follow facility policies and procedures.
- Late entry documentation: Circle the date box with your initials and you MUST document in the notes section of the MAR.
Medication Administration Records should be developed per agency-specific protocol. In some instances, pharmacies may generate medication administration records for facilities who administer an abundant amount of routine and/or PRN medications.
Routine Medication Administration Record(contains ongoing medication orders; i.e. medicines are given on a daily basis. Also contains medication that is ordered on a one time only basis.) The following are examples of information to include on the MAR:
- Month and year that the Medication Administration Record represents.
- Date order was given, and date and time medication was administered.
- Initial of the person transcribing the order.
- Initial of the person giving the medication
- Name of medication, dosage, route, time,
- An area for staff signatures, initials or other means for agency-specific staff identification.
- Acronyms are used to describe the reasons why medications were not given. See agency-specific policy regarding approved acronyms.
- Sample acronyms describing reasons why medications were not given
– R=refused
– H=hospital
– D=destroyed
- Client identification
- A most common method used for identifying residents before administering medications is photographs of residents in the medication administration records;
- Photos should be kept updated and photograph is to have the name of the resident on it
(Relying on other staff to identify residents for medication administration is not appropriate).
- Name;
- number (if applicable);
- date of birth;
- gender;
- height;
- weight.
- ALLERGIES (list in RED)
- Attending Practitioner
- Nutritional Information
- Other necessary medical information (i.e. seizure disorder, allergies, asthma, pregnancy);
- Other necessary behavioral information (i.e. checking, binging, purging, etc.).
- special diet;
- illness;
- food allergies;
Documentation for PRN medications is different.
PRN (when necessary) Medication Administration Record(contains medications that have been ordered on an “as-needed basis”). PRN medications are given on an as-needed basis per the licensed practitioner’s order.
This record should contain the same information as the routine MAR. In addition, the PRN MAR should contain:
- Documentation of time and amount administered;
- Ongoing observation, inquiry, and documentation some two hours after administration will determine effective or ineffective results of the medication;
- Documentation of the effectiveness of the medication;
- There are two acronyms that need to be added to the record to describe this (i.e. I=ineffective; E=effective).
Some Agencies May Have an Over The Counter Medication Administration Record.
ALL medications should have a “practitioner’s order”. Over the counter medications do not require prescriptions for purchase, but should be included on the practitioner’s standing medication order.
This record should contain the same information as on the PRN Medication Administration Record. In addition, there should be:
- Documentation of “why” the medication was given (i.e. complaints of headache).
- Initial appropriate box. Document on the reverse side (or other designated area) on the MAR the time, dose, and reason why PRN medication was administered.
- Check back with the client within 30-60 min and document the client’s status (better or worse?) on the reverse side (or other designated area) on the MAR. Contact the appropriate person if necessary, the document that you have notified the supervisor if a client is not improved.
- Psychotropic meds cannot be given PRN except in residential treatment facilities for the mentally ill or if the client understands the purpose of medication and is capable of requesting it.
-
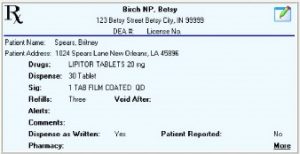
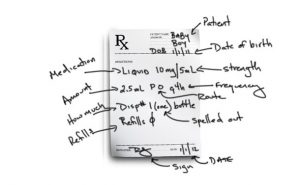
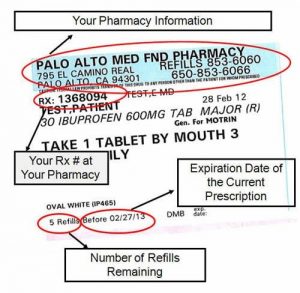
4.5. Prescription Medication Label
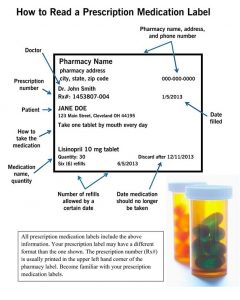
Prescription labels will contain:
- Generic and/or trade name of the medication.
- Frequency & dosage of the medication.
- Number of doses of medication that are in the package/container.
- Number of times this medication may be refilled.
- Possible food, drink, or other drug interactions
- Special instructions (i.e. allergy warnings, possible side effects, etc.)
- Name of prescribing licensed practitioner
- Expiration date
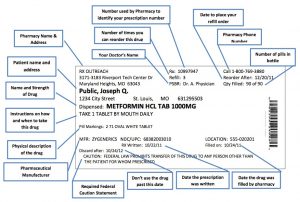
- Medication strength;
- Dispensing date;
- Directions for use;
- A pharmacy that dispensed the medication;
- Prescription number;
- Equivalency statement (when the brand or medication name dispensed is different from the brand or medication name prescribed.
-
4.6. The difference between the expiration date and the refill through date
- Expiration date – the date on the actual container, or one year after medication with no date, was filled.
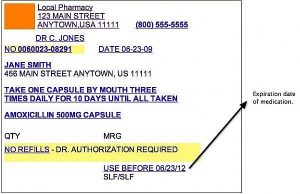
- Refill through date = is variable and determined by the prescribing authority
- Labeling requirements for over-the-counter (OTC) medications include in the original manufacturer’s bottle with the resident’s name, OR Labeled by the pharmacy;
- Prescription labels should be clear and concise and abbreviations should be discouraged for client safety in medication administration;
- It is recommended that all agencies have a list in place of what they consider approved and unapproved medical abbreviations;
- You cannot alter a medicine label.
NOTE: Medication Labels cannot be altered, they must be re-written.
- Directions on medication labels from pharmacy are checked against the MAR.
- If there is a discrepancy between the information on the MAR and the medication label, check the order in the resident’s record. (The label on medication cannot be changed by anyone. If the licensed practitioner changes the dosage on prescribed medication, a new prescription must be filled by the pharmacy. The old medication cannot be administered and must be discarded per agency policy.)

The prescription from the licensed practitioner, the label on the medication, and the information on the MAR must match exactly.
-
4.7. Summary

The MAR and the Medication Label - The QMAP uses the MAR every time when preparing and administering medications
- Do Not Ever Give Medications From Memory!!!
- Compare the medication label to the MAR three times to make sure the medication is labeled for this client and that it is the right medication, right dose, right route and the right time
- The first check happens when removing the medication container from where it is stored;
- The second check happens just before or after opening the medication and preparing it for the client;
- The third check happens after pouring the medication and before the medication is given to the client;
- The MAR is designed to promote safe and accurate medication administration;
- Information on the MAR must be clearly written and kept updated;
- The information on the MAR and the medication label should match unless there has been a change in directions
- The QMAP must be familiar with the adult care home’s policy on direction changes;
- A medication label should only be changed or altered by the dispensing practitioner Timing of Medication Administration;
- Important to understand timing in relation to administering medications, i.e., insulin and medications ordered to be administered on an empty stomach or in relation to meals;
- Timing of medications in relation to meals;
- Before meals – medication generally administered within 30 minutes prior to the resident eating meals;
- With meals – medication generally administered when the resident is eating meals or right after finishing meals;
- After meals – medication administered after the resident has finished eating meals up to 30 minutes afterward
- Clients in the facility during the medication pass should receive their medications within a window of time one hour prior to and one hour after the scheduled administration time on the MAR, except in the case of medications prescribed for administration in relation to meals or medications such as insulin;
- If unsure about giving a medication because it is outside the designated time frame;
- Contact a supervisor or a health care professional regarding the administration of the client’s medications or to determine if prescribing practitioner should be contacted;
- The medication should not be omitted without contacting a supervisor or a health care professional or prescribing practitioner.
Documentation of Medication Administration - The MAR has space where the QMAP is to initial that a dose is given under the correct day and time;
- The MAR is signed or initialed immediately after the medications are administered and prior to the administration of the next client’s medications;
- Sign or document on the MAR only after observing the client take the medications;
- Pre-charting is not permitted and this includes signing the MAR any time prior to the
medications being administered;
- Document an equivalent signature to correspond with the initials used on the MAR;
- Do not erase or cover errors. If an error is made in the documentation on the MAR, follow the facility’s policy to correctly document medication errors.

Documentation of PRN Medications - Include the amount administered, the time of administration and the reason for
Administration;
- The reason a PRN medication is to be administered is to be indicated in the order
Document effectiveness of the medication when determined;
- A different employee, depending on time of administration and shift schedules may.
MAR example.
-
4.8. Quiz 4 (check yourself)
1. List the parts of a medication order:
1________2_________3_________4_________5_________6_________7_________8_________.
2. Try to read a medication order. Can you transcribe this order into MAR?
Yes_____. No______.
3. If an order is not complete or clear on how to administer, the QMAP must contact supervisor or physician – DON’T GUESS!
True or False.
4. When the medication is received, you must read the _________and compare it to the _______________ and copy the information to the client’s _________.
a) MAR, label, prescription or order;
b) Prescription or order, MAR, label;
c) Label, prescription or order, MAR;
d) Name, prescription or order, MAR;
e) Date, prescription or order, MAR;
5. What does it mean when a medication is PRN?
a) It is to be given immediately;
b) It is to be given once a day;
c) It is to be given only with meals;
d) It is given as needed.
6. The MAR states “Seroquel 50mg, one tablet by mouth daily.” The label on the medication states “Seroquel 50mg, two tablets by mouth daily.” What should you do?
a) Give the medication as stated on the MAR;
b) Give the medication as stated on the label;
c) Check the original prescription and call the pharmacy for clarification before giving;
d) Don’t give the medication, but do leave a note for your supervisor;
e) Hold the medication until another QMAP can tell you what to do.
7. The Medication Administration Record (MAR) must have specific information on it, including:
a) The client’s weight, hair color, and identifying marks
b) The client’s food or medication allergies
c) The client’s name
d) The name of the health care practitioner who prescribed each medication listed
e) B, c, and d
Answers module 4:
1. Client’s name 2. Client’s age 3. address 4. Medication, strength 5. how much 6. instruction how to take a drug 7. A number of refills allowed 8. signature of a licensed practitioner.
2. No. 3. True. 4. c. 5. d 6.c 7. f