Communication with clients who are getting older.
The body changes with age:
This section looks at body changes. You will also learn about the changes to specific body systems and you will gain some useful information about how to provide quality care for clients who are getting older.
Visible changes.
Many visible changes take place with age. People grow shorter as the vertebrae may compress on to each other (the spinal column compresses). The density of bones decreases, mostly in women. Muscle tone and size decrease, the tendons become less flexible and cartilage deteriorates. These changes can cause a loss of flexibility and strength, changing the overall shape of a person’s body. Wrinkles, drier skin, decreased amounts of scalp hair and a reduction in the level of pigmentation in the skin are all common in the elderly. The skin also becomes less elastic; in other words, it doesn’t have as much stretch as younger skin. An older person’s skin gets thin, making it easier to bruise, scratch or tear. Older people perspire less, hair becomes gray and the finger and toenails grow more slowly, showing some discoloration and lines.
Sensory changes.
Many sensory changes occur with aging. Hearing loss occurs. Sounds in the higher frequency range (such as high-pitched voices) are lost first, and sounds must be louder to be heard. Hearing problems can contribute to isolation, anxiety and depression in the older adult and can result in behavior problems. The client may withdraw from gatherings rather than strain to listen.
As a direct care staff person, communicating with clients who suffer from a hearing loss can be difficult, but using the following ideas will make your job easier:
- Make sure that if clients wear hearing aids, they are in and the batteries are working.
- If they don’t wear a hearing aid you can do the following to communicate:
- Face the person and get their full attention before you talk.
- Decrease noises.
- Speak clearly and slowly.
- Speak at a lower pitch or your normal pitch.
- Use pleasant facial expressions and gestures.
- Remove gum and candy from your mouth.
- Keep your hands away from your face in case they follow your lips to understand what you are saying.
- Allow time between sentences and rephrase sentences if necessary.
- Use a pad of paper to write notes.
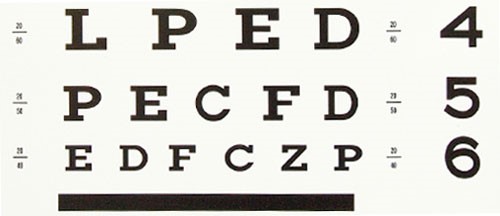
Vision, like hearing, is another common change in older adults. Normal changes in vision include the lack of ability to see close and read. Larger print is helpful. Older persons also do not see as well at night. In general, older adults see better with twice the light that they may have needed in the past. If the light seems very bright to you, it may be just at the limit of what the older person needs to be able to see. Make sure to avoid glare however, as this will interfere with vision too.
Sensitivity to smell and taste decrease with age. Older persons cannot taste foods the way they used to taste. This can lead to less interest in eating. If an older adult client has less pleasure when eating, this may affect what he/she eats. An older person may have a reduced appetite and weight loss. If he/she is not getting proper nutrition it may affect other body functions such as healing of wounds. Not all taste abilities decline at the same rate. The sensitivity to the taste of salt does not decrease as much as sensitivity to some other tastes, such as to sweet foods. The concern here is that this can lead to clients eating more salt than they need, and this can lead to excess fluid retention.
The sense of touch changes. In older adults the sense of touch may decrease as skin loses sensitivity. Pressure, pain, cold and heat do not feel the same as they used to feel. Decreases in touch sensitivity may cause clients to drop things. An older adult client may not notice the temperature of water, so he/she can get burned more easily. You may find that you must frequently check the temperature of things before a client comes into contact with them. As a direct care staff person, watch for skin discoloring that is white or purple in color, open areas and for skin that is cooler to the touch.
Cardiovascular system. This system includes the heart, lungs and the blood vessels. Circulation of the blood slows down; this can result in older clients feeling cold, especially in the hands, feet and legs. Cuts and tears to the skin may take longer to heal and require extra care. One suggestion or guidance you can provide is to encourage the client to change positions so they are not always lying down or sitting. This will help avoid skin breakdown and increase circulation. However, be sure that changes in position are done slowly so as not to cause the client to get dizzy and fall.
Neurological system. This system includes the brain and nerve system. Cells in the brain that are lost do not reproduce, and up to 25% of brain mass can be lost in the aging process. Older people take longer to remember things, respond to questions and finish certain kinds of tasks. It is not a sign of less intelligence. Rather, it simply takes longer to make the connections in the brain than it did when the client was younger.
Respiratory system. This system that keeps us breathing changes with age, too. It takes longer to get better after a cold or flu. It is important to watch for and report shortness of breath and swelling in the legs or feet.
Urinary system. Prostate infections (in men) and infections in the bladder may increase, and recovery is slower. As a direct care staff person, to reduce the risk of bladder infections, teach the female client to wash her private area from front to back. Watch how much the client drinks (ideally, he/she should drink eight large glasses of water a day). Encourage the client to use the toilet every two hours to reduce the risk of accidents and infections. Watch for dark, foul smelling urine and increased urinary frequency. These may be signs of a urinary tract infection that can cause pain, burning, increased confusion and behavior problems. Report any changes in urine or toileting to your supervisor.
Digestive system. This system breaks down food. Changes in the teeth and loss of teeth occur more with the elderly and can have an impact on ability to chew and digest food. If the teeth are not strong, soft food may be easier to chew. The client may need to drink more to help swallow.

Muscular-skeletal system. A client’s muscles may be weaker, joints may be sore and stiff and bones may be brittle. As a direct care staff person, you may have to assist the client in getting in and out of a chair and with activities such as dressing and walking. Encourage the client to do simple exercises to keep limber. Walking and simple exercises are excellent activities to prevent stiffness and pain.

Psychological issues and aging:
Older people must make many adjustments. Often these adjustments are handled without any problem and the quality of life stays high. Less often, people struggle, and in some cases experience stress that reduces their quality of life. Older persons may feel afraid, confused, nervous or helpless. Generally, these reactions happen when there is a sudden and unusually negative change in the person’s life situation. When you observe any of these reactions, report them to your supervisor immediately.
It is normal for any of us to be temporarily depressed over a loss, and this is true for an older adult. Over time we adjust and this situational depression lifts. However, depression that continues without improvement is not a normal part of aging, and it can be quite serious. People who are depressed have a much higher risk of suicide. Because depression is treatable, it is important to recognize its symptoms and report them to a supervisor who can arrange for an assessment.

The symptoms for depression include: sadness, guilt, a sense of worthlessness, hopelessness, fatigue, tearfulness, weight loss, irritability, excessive complaints of aches and pains that have no apparent cause, anger and sleep disturbances. One of the things that makes it harder to recognize depression is that it can often occur with other diseases or conditions such as dementia, heart disease, Parkinson’s disease, stroke, diabetes and cancer. When this happens it is easy for people to assume that it is normal for someone with one of these conditions to be depressed. This is dangerous thinking and is not true. Despite having another illness, someone who is depressed should be treated for the depression along with treatment for other illnesses.