7. Principles of basic nutrition to client care.
-
Principles of nutrition needs.

An essential nutrient is a nutrient that the body cannot synthesize on its own — or not to an adequate amount — and must be provided by the diet. These nutrients are necessary for the body to function properly. The six essential nutrients include carbohydrates, protein, fat, vitamins, minerals and water.
Carbohydrates
Carbohydrates are the main energy source for the brain. Without carbohydrates, the body could not function properly. Sources include fruits, breads and grains, starchy vegetables and sugars. Make at least half of the grains you consume whole grains. Whole grains and fruit are full of fiber, which reduces the risk of coronary heart disease and helps maintain normal blood glucose levels.

Carbohydrates can be grouped into two categories: simple and complex. Simple carbohydrates are sugars whereas complex carbohydrates consist of starch and dietary fiber. Carbohydrate provides about 4 kcal (kcal = kilocalories = Calories) per gram (except for fiber) and is the energy that is used first to fuel muscles and the brain. Soluble fiber (fruits, legumes, nuts, seeds, brown rice, and oat, barley and rice brans) lowers blood cholesterol and helps to control blood sugar levels while providing very little energy. Insoluble fiber (wheat and corn bran, whole-grain breads and cereals, vegetables, fruit skins, nuts) doesn’t provide any calories. It helps to alleviate digestive disorders like constipation or diverticulitis and may help prevent colon cancer. Most calories (55-60%) should come from carbohydrates. Sources of carbohydrates include grain products such as breads, cereals, pasta, and rice as well as fruits and vegetables.
Protein
Protein is the major structural component of cells and is responsible for the building and repair of body tissues. Protein is broken down into amino acids, which are building blocks of protein. Nine of the 20 amino acids, known as essential amino acids, must be provided in the diet as they cannot be synthesized in the body. Ten to 35 percent of your daily calories should come from lean protein sources such as low-fat meat, dairy, beans or eggs.
Protein from food is broken down into amino acids by the digestive system. These amino acids are then used for building and repairing muscles, red blood cells, hair and other tissues, and for making hormones. Adequate protein intake is also important for a healthy immune system. Because protein is a source of calories (4 kcal per gram), it will be used for energy if not enough carbohydrate is available due to skipped meals, heavy exercise, etc. Main sources of protein are animal products like meat, fish, poultry, milk, cheese and eggs and vegetable sources like legumes (beans, lentils, dried peas, nuts) and seeds.
Fat
Fat is an energy source that when consumed, increases the absorption of fat-soluble vitamins including vitamins A, D, E and K. Twenty to 35 percent of your daily intake should come from fat. Choose healthy options such as omega-3-rich foods like fish, walnuts and vegetable-based oils. Omega-3s help with development and growth. Limit intake of saturated fats such as high-fat meats and full-fat dairy. Other smart choices include nuts, seeds and avocado.
The fat in food includes a mixture of saturated and unsaturated fat. Animal-based foods such as meats and milk products are higher in saturated fat whereas most vegetable oils are higher in unsaturated fat. Compared to carbohydrate and protein, each gram of fat provides more than twice the amount of calories (9 kcal per gram). Nevertheless, dietary fat does play an important role in a healthy diet. Fat maintains skin and hair, cushions vital organs, provides insulation, and is necessary for the production and absorption of certain vitamins and hormones. Nutrition guidelines state that Canadians should include no more than 30% of energy (calories) as fat and no more than 10% of energy as saturated fat.
Vitamins
Vitamin C is necessary for the synthesis of collagen, which provides structure to blood vessels, bone and ligaments. Rich sources include citrus fruits, strawberries and peppers. Folate, found in foods, helps to prevent birth defects. Pregnant women or women who plan to become pregnant should speak with their physician about taking a folic acid supplement, the synthetic form of folate, in addition to their diet. Vitamin D helps to maintain calcium homeostasis. It can be found in food sources or synthesized by the sun. Vitamins help to regulate chemical reactions in the body. There are 13 vitamins, including vitamins A, B complex, C, D, E, and K. Because most vitamins cannot be made in the body, we must obtain them through the diet. Many people say that they feel more energetic after consuming vitamins, but vitamins are not a source of energy (calories). Vitamins are best consumed through a varied diet rather than as a supplement because there is little chance of taking too high a dose.
Minerals
Sodium helps to maintain fluid volume outside of the cells and helps cells to function normally. Keep intake under 2,400 milligrams per day. Potassium maintains fluid volume inside and outside of cells and prevents the excess rise of blood pressure with increased sodium intake. Rich sources include bananas, potatoes and tomatoes. Calcium helps to maintain and build strong bones and teeth. Include three servings of calcium-rich foods per day including milk, low-fat cheese and yogurt.
Minerals are components of foods that are involved in many body functions. For example, calcium and magnesium are important for bone structure, and iron is needed for our red blood cells to transport oxygen. Like vitamins, minerals are not a source of energy and are best obtained through a varied diet rather than supplements.
Water

Water helps to maintain homeostasis in the body and transports nutrients to cells. Water also assists in removing waste products from the body. All beverages and high-moisture foods such as soup and watermelon contain water and count towards your daily water requirement. Adults should consume 25 to 35 milliliters of fluids per kilogram body weight or 2 to 3 liters per day.
Water is a vital nutrient for good health. Most of our body weight (60-70%) is made up of water. Water helps to control our body temperature, carries nutrients and waste products from our cells, and is needed for our cells to function. It is recommended that adults drink 8 glasses of fluid daily (or more in hot weather or during physical activity). This fluid does not have to be water alone. It can also be obtained from juice, milk, soup, and foods high in water such as fruits and vegetables. Caffeine-containing beverages (coffee, tea, and cola) don’t count because caffeine is a diuretic, making us lose water. A great plus for water in comparison to the other fluids is that it hydrates our body without extra calories.
Minerals are components of foods that are involved in many body functions. For example, calcium and magnesium are important for bone structure, and iron is needed for our red blood cells to transport oxygen. Like vitamins, minerals are not a source of energy and are best obtained through a varied diet rather than supplements.
-
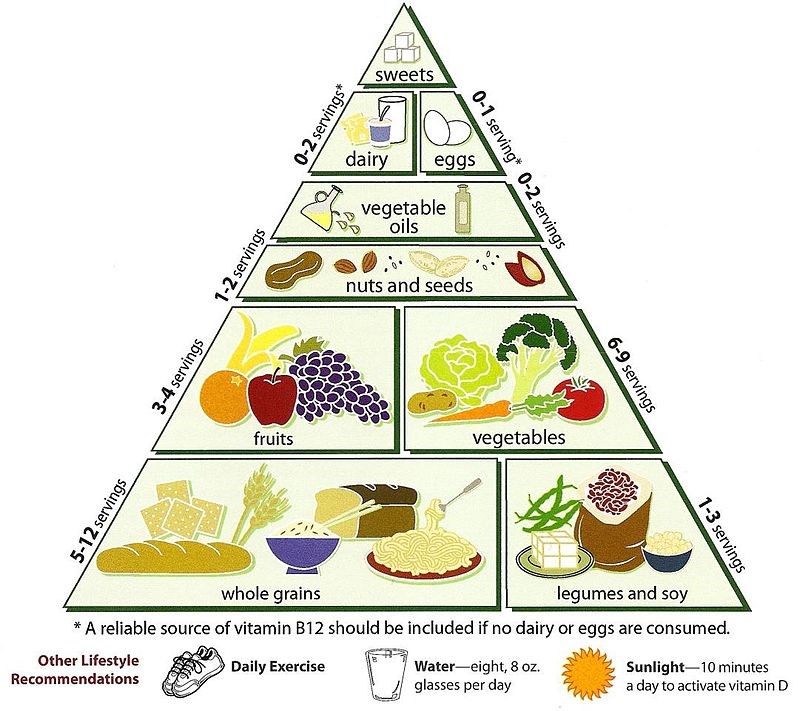
Food Pyramid.
The Food Pyramid, developed by the US Department of Agriculture (USDA), is an excellent tool to help you make healthy food choices. The food pyramid can help you choose from a variety of foods so you get the nutrients you need, and the suggested serving sizes can help you control the amount of calories, fat, saturated fat, cholesterol, sugar or sodium in your diet.
Suggested Servings from Each Food Group

The American Heart Association recommends eating a healthy diet full of fruits, vegetables, whole grains, and other nutritious foods.
This table shows the suggested number of servings from each food group based on a daily intake of 1,600 or 2,000 calories.
There is a right number of calories for you, depending on your age, physical activity level and whether you are trying to lose, gain or maintain your weight. Use our Fats and Sodium Explorer tool to get your personal daily calories.
Food Type 1,600 Calories 2,000 Calories Examples of One Serving Grains
At least half of your servings should be whole-grain.6 servings per day 6-8 servings per day 1 slice bread1 Oz dry cereal (check nutrition label for cup measurements of different products)1/2 cup cooked rice, pasta, or cereal (about the size of a baseball) Vegetables
Eat a variety of colors and types3-4 servings per day 4-5 servings per day 1 cup raw leafy vegetables (about the size of a small fist)1/2 cup cut-up raw or cooked vegetables1/2 cup vegetable juice Fruits
Eat a variety of colors and types4 servings per day 4-5 servings per day 1 medium fruit (about the size of a baseball)1/4 cup dried fruit1/2 cup fresh, frozen, or canned fruit1/2 cup fruit juice Fat-free or low-fat dairy Products 2-3 servings per day 2-3 servings per day 1 cup fat-free or low-fat milk1 cup fat-free or low-fat yogurt1 and 1/2 oz. fat-free or low-fat cheese (about the size of 6 stacked dice) Lean meats, poultry, and seafood 3-6 oz. (cooked) per day Less than 6 oz. per day 3 oz. cooked meat (about the size of a computer mouse)3 oz. grilled fish (about the size of a checkbook) Fats and oils
Use liquid vegetable oils and soft margarine most often2 servings per day 2-3 servings per day 1 Tsp. soft margarine1 Tbsp. mayonnaise1 Tsp. vegetable oil1 Tbsp. regular or 2 Tbsp. low-fat salad dressing (fat-free dressing does not count as a serving) Nuts, seeds, and legumes 3-4 servings per week 4-5 servings per week 1/3 cup or 1 and 1/2 oz. nuts2 Tbsp. peanut butter2 Tbsp. or 1/2 oz. seeds1/2 cup dry beans or peas Sweets and added sugars 0 servings per week 5 or fewer servings per week 1 Tbsp. sugar1 Tbsp. jelly or jam1/2 cup sorbet and ices1 cup lemonade -
Personal Preferences for food based on personal and cultural choices.
Food allergies or food intolerances affect nearly everyone at some point. People often have an unpleasant reaction to something they ate and wonder if they have a food allergy. One out of three people either say that they have a food allergy or that they modify the family diet because a family member is suspected of having a food allergy. But only about 5% of children have clinically proven allergic reactions to foods. In teens and adults, food allergies occur in about 4% of the total population.

Introduction

Effective care doesn’t happen in isolation. You are part of a team of care workers who work together to meet individuals’ needs. One area where you will need to work closely with other members of staff is in providing the right diet to suit both your client’s individual likes and dislikes and to meet any cultural preferences they may have.
Why diets are important
Diet does not mean reducing your fat or carbohydrate intake to lose weight, though such diets do, of course, exist. A person’s diet simply means the type of food they eat.
A client’s diet will be influenced by their culture – their beliefs and values. These may in turn be influenced by their religion or ethnic background. Individual preferences, such as always eating the main meal of the day in the evening or having Sunday lunch with the family, are part of people’s individual cultures and are equally important.
When a person is admitted into care, it is important to find out their likes and dislikes, their normal pattern of eating and any specific needs they may have. This will help to achieve an environment that promotes choice and demonstrates respect for an individual’s personal beliefs and preferences.
“I remember nursing a resident who had her food liquidized; she had no speech and a very poor swallow reflex. She did not seem to enjoy her main course at all. It wasn’t until I had mentioned this to her daughter that I found out that the resident in question never used to mix her dinner when she ate it: she would eat all the vegetables except the potato first, then the potato and finally the meat.
Once this resident’s food was liquidized separately, she began to enjoy mealtimes again. Simple things can be easily missed.”
As a Care Worker, you must show just as much respect for a client who requires their meat to be cooked in a certain way because of religious needs as for someone who always likes tomato sauce on everything. And a person who has never eaten certain vegetables because they don’t like them is as important as a vegetarian who has strong beliefs about not including meat in their diet.
-
Meeting clients’ needs.
At a team meeting organize time to discuss diet and culture with your colleagues. Identify clients in your care who have specific needs.
Try to find out more about the dietary requirements of particular religions. You could ask other people such as the chef, cook or the local dietician, or look on the internet. As you research, try to find out which of the following statements are correct.
Diet and culture
Jewish people:
- Do not eat meat;
- Do not eat chicken;
- Do not eat meat and milk together;
- Are vegetarian.
Hindus:
- Have their meat killed and prepared in a particular way (kosher)
- Do not eat meat from carnivorous animals
- Do not eat beef only eat fish.
Muslims:
- Will only eat meat killed in a particular way (halal)
- Don’t eat fish or meat
- Are vegetarian
- Do eat pork.
Sikhs:
- Do not eat beef and do not drink alcohol
- Do not eat pork or drink alcohol
- Do drink alcohol
- Only eat meat.
Vegetarians:
- Only eat organic vegetables
- Have nut loaf for Sunday lunch
- Have a protein deficient diet
- Do eat dairy products and eggs.
Rastafarians:
- Do not eat pork
- Do not eat beef
- Like their meat cooked in a certain way
- Drink milk with their meals.
Planning and monitoring
Talk to your clients and find out how their different needs are managed. Where do you record this information?
Ask your manager whether you can complete the menu request form with one client over a period of, say, 2 weeks. Check that the client is happy for you to do this. Have a look at menu; ask yourself and your client questions to help you analyze the information. The following questions may help you.
- What choices are there?
- Over a period of time what has the variety been like?
- Is the client always choosing the same thing?
- Does more choice need to be given?
- Has the client had the chance to request something different?
- Have the client’s personal beliefs and preferences been met in full?
- Is the client happy with the choices offered or do you feel that he/she is just accepting what is on offer?
- Do you feel anything more could be done?
- Complete the client’s care plan on your findings. You need to make sure your entry is correct. Remember to ask for help if you are unsure.
- Write up what you have done, what you have found out and what action you feel needs to be taken. Present this report to your manager.
Reporting
Helping a client to eat and drink their preferred food is also a very important part of a Care Worker’s role. There are many factors that need to be taken into consideration.
-
Dietary problems of seniors.
Nutrition Difficulties
Observe your care recipient closely for difficulty in eating, chewing, or swallowing. The difficulty may be caused by the muscles or nerves not working properly anymore or by the care recipient forgetting how to do it. Difficulty in swallowing is called dysphasia. Two issues are the most important if a care recipient has dysphasia: positioning and thickened fluids. The care recipient should be positioned upright as much as possible, not leaning forward or backward. Fluids should be thickened since a liquid is difficult to control and swallow in its normal state. When it is thickened, it is easier to swallow. There are different consistencies that may be ordered, such as nectar, honey, or pudding. There are several commercial powders you can buy to thicken fluids and there are prepared products you can purchase. The care recipient may need foods that are easier to chew and swallow. He/she may need more supervision with eating so direction can be provided by the caregiver.
Age related factors that influence adequate dietary intake:
- Loss of appetite;
- Reduced sense of taste;
- Loss of dentation;
- Denture problems;
- Dehydration;
- Malnutrition;
- Severe weight loss;
- Severe weight gain
Situational factors:
- Ileostomies;
- Dysphagia;
- Confusion;
- Medications;
- Depression;
- Grief;
- Immobility;
- Medical problems.
Aspects of personal care worker care:
- Socialization;
- Atmosphere;
- Presentation of food;
- Variety of seasonings;
- Oral inspection and hygiene;
- Denture care;
- Adequate fluid intake using a variety of fluids;
- Comfort foods;
- Thickened liquids;
- Liberalized diets – comfort foods;
- Adequate Hydration.
Ensuring Adequate Hydration in the Elderly
According to the Journal of the American Geriatrics Society, dehydration is the most common fluid and electrolyte disorder in the elderly with a prevalence of 20-40%.The elderly are at a high risk for dehydration related to a decreased sense of thirst, fear of being incontinent, swallow difficulties and gastrointestinal disorders just to name a few. Fluid intake reduces as the aging process takes place. Dehydration in the elderly is associated with a higher complication rate and must be regularly monitored. Standard follow-up from nursing and dietary paired with client education on strategies to maintain adequate hydration levels are essential to preserve optimal hydration in the elderly population. The importance of adequate hydration among the elderly cannot be stressed enough. There are several ways to ensure adequate fluids are being consumed by our elderly clients:
- Keep a full and fresh water pitcher at the bedside table.
- Ensure the water pitcher and a cup is within the client’s reach.
- Incorporate foods high in water content (e.g. popsicles, gelatin and watermelon) in daily activities.
- Make drinks more appealing by using lemonade pitchers and glasses, cocktail decorations or a fruit garnish.
- Take a proactive approach when administering fluids. Hand the clients a drink as opposed to asking if they want a drink.
- Identify clients at high risk for dehydration and place a symbol (e.g. a picture of a water droplet) in the client’s rooms to remind family or client to encourage fluid consumption.
- Provide a variety of sugar-free flavored beverages, such as Crystal Light, to help increase palatability and assist with hydration.
- Have the Dietitian re-evaluate the clients on fluid restrictions. He/she can make recommendations, if appropriate, to liberalize the restriction.
- Provide client education about the importance of adequate hydration.
Monitoring Hydration Status and Recognizing Dehydration
On a daily basis, most people get enough fluid through normal drinking behavior, such as drinking with meals and snacks. However, thirst isn’t always a reliable gauge of hydration status, especially in children and older adults. A better barometer is the color of the urine. For most healthy individuals, clear or light-colored urine suggests adequate hydration, whereas a dark yellow or amber color usually signals dehydration, although certain medicines and vitamins may cause the color of the urine to change, making this test unreliable. Infrequent urination and low urine volume can also suggest inadequate hydration.
Mild dehydration can affect physical and mental performance and contribute to unpleasant physical symptoms like headaches and muscle cramps. The early signs of dehydration can be non-specific, usually involving fatigue, headache and confusion. Oral rehydration is usually all that is required. But because severe dehydration can be life threatening, medical help should be sought quickly if there is any concern about someone needing more aggressive fluid supplementation. However, severe dehydration can be life threatening.
Because dehydration can develop quickly under some conditions, it’s important to recognize the following signs of dehydration in others and act quickly to help them cool down and rehydrate.
Signs of Dehydration
- Increased thirst
- Dry or sticky mouth
- Light-headedness or headache
- Fatigue
- Impaired mental focus
- Low urine output
- Inability to produce tears
- Dry skin
Measuring intake and output.
- Intake – oral and food;
- Output
-
Intake And Output (I&O), Personal care worker responsibilities to promote adequate fluid and food intake.
Intake and output (I&O) is the measurement of the fluids that enter the body (intake) and the fluids that leave the body (output). The two measurements should be equal. (What goes in…. must come out!)
The metric system is used for fluid measurement. The measurements should be recorded in ml. (Milliliters).
The average adult intake is 2500-3000mL. Per day.
The average output is 2500-3000mL. Per day.
Common metric conversions used for I&O:
1 c.c. = 1 ml 1 ounce = 30 ml. 1L. = 1000 ml.
To convert from ounces to ml. multiply by 30 (Ex. 6 oz. x 30ml. = 180ml.)
To convert from cc/ml to ounces, divide by 30 (Ex. 240cc / 30cc = 8 oz.)
Sizes of containers vary. Know your facility’s container measurement system.
INTAKE & OUTPUT: Metric Conversions
Using the basic volume conversions, convert the following equations to the metric system.
Basic conversions:
1 ml. = 1 cc.
1 ounce (oz.) = 30 ml.
1 cup = 8 oz.
1 pint = 2 cups
Hints:
To convert from ml. or cc. to ounces, divide by 30.
To convert from ounces to ml. or cc., multiply by 30.
Conversions:
- 1 cc. = ml.
- 2 oz. = ml.
- ½ oz. = ml.
- 4 cc. = ml.
- 8 oz. = ml.
- 6 oz. = ml.
- 4 oz. = ml.
- ½ cup = oz. = ml.
- 2 (8 oz.) cups of coffee = ml.
- 1 (6 oz.) bowl of broth = ml.
- 3 (8 oz.) glasses of water = ml.
- 2 (4 oz.) glasses of ice chips = ml.
- 2 (4 oz.) dishes of gelatin= ml.
- ½ pint of milk = ml.
Nutrition and Fluid Balance
Convert the following measurements.
- 30ml. = oz.
- 2 oz. = ml.
- 2 (8oz.) cups of coffee = ml.
- 1 (6 oz.) bowl of soup = ml.
- 3 (8 oz.) glasses of water = ml.
- 2 (4 oz.) glasses of ice chips = ml.
- 2 (4 oz.) cups of gelatin = ml.
- 100% (6 oz.) bowl of soup = ml.
- 75% (8 oz.) cup of coffee = ml.
- 50% (4 oz.) cup of gelatin = ml.
- 10% (6 oz.) bowl of soup = ml.
- ¼ (4 oz.) cup of gelatin = ml.
- ½ (6 oz.) bowl of soup = ml.
- ¾ (8 oz.) cup of water = ml.
Sources of fluids:
- Oral fluids;
- Food;
- Intravenous fluids.
Sources of fluid excretion:
- Lungs;
- Skin;
- Kidneys;
- Intestines.
Personal care worker responsibilities to promote adequate fluid and food intake.
Tasks that may be performed by the personal care worker to promote adequate fluid and food intake
- Before meal hygiene;
- Position of client to prevent aspiration;
- Serving food trays;
- Feeding a client;
- Use of assistive devices for feeding/drinking;
- Adequate fluids intake or restricting fluids as ordered;
- Encouraging independence while feeding/drinking;
- Post meal hygiene.
Assistance with mealtime:
Many of the tasks with which you will help clients have been studied and analyzed to find safe, respectful and effective ways for you to assist the client. In this module you will be introduced to ways to assist someone with eating. The assistance with mealtime can be broken into areas. Each is presented below along with the steps to accomplish it.
- 1. Preparing the resident to eat.
For most people, eating is a social event. That is, it is often done with other people. For some clients it may be one of the more important times of the day when they interact with others. So, it is important to help prepare clients for meals. Here are some ways in which you can help:
- Ask the client if he/she would like assistance in brushing his/her hair or putting on make-up.
- Ask the client if he/she needs to use the bathroom. Assist the client according to his/her needs.
- Assist the client in washing his/her hands or face if assistance is needed.
- Ensure that the client has his/her dentures on if they wear them.
- Ask the client where he/she would like to sit in the dining room.
- 2. Serving meals and providing assistance during meals.
As mentioned above, mealtime is an important social time. This time with others is enhanced when the atmosphere is pleasant, calm and enjoyable. While performing your tasks, keep in mind that your calm, relaxed, friendly, encouraging and helpful behavior will go a long way toward making mealtime special. Here are the kinds of tasks you may perform:
- Serve the meal to the client by calmly and quietly placing it within easy reach.
- Make sure the client has all the utensils he/she will need.
- Check the client frequently to see if he/she needs help.
- Offer to cut food for a client who is having difficulty. When cutting food, always make sure the pieces are small to help prevent choking. A client with arthritis may also need help with things such as opening milk containers.
- Offer different food if a client refuses what was offered. Each client has a right to food that is appealing and nutritionally sound.
- Allow the client time to complete one course before starting another.
- If you see any of the following, tell your supervisor:
- A change in the amount of assistance a client needs while eating.
- A change in general behaviors during mealtime such as playing with food, taking food from others, throwing food or falling asleep.
- A change in attitude such as withdrawing, showing anger or frustration.
- Choking while eating or drinking.
- Eating less or more food than usual.
- A refusal to eat.
- Wait for all client to complete their meal before starting another activity or turning on a dishwasher.
- If needed, help the client check their personal appearance before moving away from the table. For example, check to see if there are any food spills or crumbs that need to be cleaned. Help a client to wipe his/her face, if necessary.
In addition to the basic steps already listed, several other things should be considered. First, it is important that the clients’ cultural preferences and beliefs be considered. For example, you may have a client who wants to pray before each meal. While you do not have to pray with the client, it is important that you sit quietly and respectfully while the client does this. You should also be sensitive to the fact that many people’s food preferences are strongly influenced by their culture, ethnic background and religion. These preferences should be honored when possible.
You may also have responsibilities to help prepare the dining room for meals. You might be involved in removing clutter or hazards, reducing distractions such as loud noise or cleaning the table. You may also encounter client who don’t eat at times pre-set by the personal care. For example, you may have a client who likes to wake up at 10 a.m. and have a light breakfast of fruit and coffee instead of the 8 a.m. breakfast call. Honor preferences by being flexible.
-
Assist Dependent Clients With Eating.
Weakness, paralysis, casts, and other physical limitations may make self-feeding impossible. The family caregiver needs to handle this situation professionally. Sometimes, it is hard for care recipients to accept the idea of not being able to feed themselves. They may feel resentful and depressed. Remember to be friendly and to encourage them to do as much as possible for themselves. Before serving a meal, remember the following:
- Offer the care recipient the opportunity to toilet. If the client has been incontinent, change the person before serving food.
- Offer the care recipient oral hygiene.
- Help the care recipient to wash hands and face.
- Make sure the care recipient is comfortable and positioned properly (upright at 45-90 degrees with the head stabilized).
- If the care recipient has dentures, make sure they are in.
- Protect the care recipient’s clothing, if necessary. A towel or special protector can be used. Do NOT refer to it as a ‘bib.’ Instead, call it an apron, clothing protector, or cover-up.
- Be familiar with client’s diet and any restrictions (e.g. calories, sweets, salt).
During a meal, follow these guidelines:
- Sit down beside the care recipient, at the same level.
- Carry on a pleasant conversation with the care recipient.
- Don’t rush the care recipient. Feed slowly and carefully.
- Pick up eating utensils by the handles.
- Avoid touching the food if you can.
- A spoon may be safer to use than a fork.
- Explain to the client what you are going to do, and what foods are on the tray, and ask what he or she would like to eat first.
- Make sure the person’s mouth is empty before offering the next bite of food or sip of beverage.
- Make sure the food is not too hot.
- Allow time for the client to chew and swallow, and watch for signs of gagging and chocking.
- Offer beverages throughout the meal; use a straw for liquids if necessary. Be careful of temperature of liquids.
- Stop feeding when the client does not want more or seems tired.
- For feeding a blind client, describe the food you are offering and use the numbers on clock to identify the location of the food on the plate.
After the meal, follow these guidelines:
- Assist the care recipient to wash hands and face.
- Assist the care recipient with oral hygiene, if desired.
- Assist the care recipient to a comfortable position.
- Refrigerate leftovers and clean up eating area.
- You may wash dishes at this time.
- If the care recipient routinely doesn’t eat well, you may want to report it to the care recipient’s physician.
-
Meal Planning and Preparation, Food Handling and Storage.
MEAL PLANNING AND PREPARATION
As a personal caregiver, you may have to purchase food for your client. First, develop a menu of what foods will be prepared. Check the ingredients the care recipient has on hand and make a shopping list. A list will help avoid unnecessary trips to the store for forgotten ingredients. It will also prevent duplicate buying of foods already on hand, and, if grouped by types of food, avoid extra steps in the grocery store. Things to remember when planning a meal:
- Variety – A well-balanced diet consists of getting nutrients from many different kinds of foods. No one food is perfect.
- Texture – Combining crispy foods with smooth, soft ones make each texture seem more interesting. Unless the care recipient is on a special diet where the texture of the food is controlled, try to choose different types of texture within each meal served.
- Flavors – If all foods in the meal have a strong, distinctive taste, they will compete with one another and overwhelm the care recipient’s taste buds. Keep the strong flavored foods as the spotlight with milder tasting foods as the background.
- Color – Give each meal an appealing look by keeping the colors compatible. A sprig of parsley, radish roses, olives, or carrot curls may make an interesting dash of color to an otherwise drab-looking meal.
- Cost – Most elders are not free to spend an unlimited amount of money on their food, so plan meals that are within their budgets. Consider foods on sale and use coupons whenever possible.
Shopping
Occasionally, clients will ask employees to go shopping for them. Check with the office to get approval, unless running errands is written in the Plan of Care.
Assisting with Shopping:
- Review the Grocery List.
- Inventory items on hand or needed, such as basic food, paper goods, toiletries, and cleaning supplies.
- Familiarize yourself with sale items at the grocery store or review newspaper ads with the client.
- Obtain specific information regarding each Item: size, quantity, color, ripeness, and cost.
- Ask the clients about buying a comparable sale item if it’s cheaper.
- Pick up perishables last stop in the grocery store, especially in hot weather.
- Get groceries home and refrigerate perishables as quickly as possible.
- Don’t leave perishables in the car while you run other errands.
- If you live more than 30 miles from the store, consider using an ice chest.
When you shop, be careful in the selection of perishable foods.
- Make sure that frozen foods are solid and that refrigerated foods feel cold.
- The “sell by” and “use by” dates are printed on many perishable foods.
- Pay attention to expiration dates on sealed, canned, and bottled items.
- The “sell by” date tells grocer and buyer how long produce should be kept for sale on the shelf.
- The “use by” date is indicates how long the food will retain top eating quality after purchase.
Money Handling Techniques:
- Count the money in front of the client before leaving the home.
- Place the client’s money, grocery list, coupons, and food stamps in an envelope, zip-lock bag, or separate coin purse.
- Upon return, give the client receipts, return unused coupons, and count the change for the client.
- Whenever possible, use a store that itemizes receipts.
Storage of Items Purchased:
- Follow client instructions.
- Be aware of client limitations:
- Label items.
- Open jars ‘and milk cartons as needed.
- Store items properly.
- Re-package items into smaller portions as needed.
Meal Shopping/Purchasing It is important to READ labels when purchasing packaged food, as the listing of ingredients on these labels is critical for special diets. Those on salt-free diets, for example, must avoid products that list sodium on the labels. Likewise, diets that restrict the use of sugar can avoid sugar by checking the label. People with allergies to certain types of foods or chemicals can use the ingredient panel on a label when planning what to eat. Labels also tell us the amount of food in the container, and, sometimes, the number and amount of servings, as well as the calories per serving. This could be important to those care recipients on a low calorie diet. The label may also list the kind of nutrients in the food and the amounts of the nutrients. In products that contain more than one ingredient, such as spaghetti in meat sauce, all the ingredients must be listed. The ingredients found in the greatest amount will be listed first. The ingredient listed last would have the smallest amount. Convenience foods usually cost more than foods prepared from scratch. You must consider that ingredients might spoil before they are completely used. Deciding what to purchase must be made on an individual basis. Purchasing larger quantities can be cheaper than buying small quantities of an item. If storage is a problem, however, the item may have to be discarded before it is all used. Discuss the amount of ingredients needed with your care recipient before you go to the store. Consider the cost of seasonal foods when purchasing foods. Foods that are in season are usually a good buy.
Here is how to reduce the cost of foods that are high in protein:
- Use poultry when it is cheaper than red meat.
- Consider cuts of meat that may cost more per pound but give more servings per person.
- Learn to prepare less tender cuts of meat in casseroles or pot roasts.
- Serve egg dishes such as omelets. # Substitute dried bean and pea dishes for higher cost meals.
- Use fillers such as breadcrumbs or pasta to make a meat dish serve more.
FOOD HANDLING AND STORAGE
Kitchen Food Safety
Food Safety Infection Control in the Kitchen
- It is very important for the home care worker to understand how to prepare and store foods in a safe manner.
- Foods can be contaminated (poisoned) in different ways.
Anyone who prepares and/or handles food should follow these guidelines.
- ALWAYS WASH YOURHANDS BEFORE HANDLING FOODS.
- Keep your hair pulled back or covered. Stray hair is a contaminant.
- Foods like raw meats, fish, and eggs can naturally harbor harmful bacteria or parasites. Cooking these foods thoroughly will solve this problem.
- Other foods are contaminated because of improper handling and storage.
- Avoid letting foods stay at room temperature.
- Keep HOT-foods HOT, and keep COLD-foods COLD.
- Wash all fresh fruits and vegetables.
- Rinse meats before cooking.
- Use disinfectants on surfaces.
- Wash tops of cans before opening.
- Keep surfaces and utensils clean, such as:
- Countertops, cutting boards, can openers, dishes, pots and pans;
- Sponges, dishcloths, dishtowels;
- Trash cans, appliances, and telephones.
WASH HANDS FREQUENTLY.
Nutritious Meal Preparation
Homemakers are frequently called upon to assist clients with meal planning and preparation. The homemaker needs to be concerned with safe handling of foods (see: Kitchen Safety on previous pages) and the nutritional values of foods for clients. The “Food Guide Pyramid” has been designed as a guide for everyone to use when planning nutritious meals. There are four things to remember about a healthy diet, using the pyramid:
1. Moderation:
- Moderation refers to the amount of food needed for a health body weight.
- Some food choices contain fat or added sugar and they should be eaten in moderation.
2. Balance:
- The shape of the pyramid indicates that grains, fruits, and vegetables should make up most of our daily calories. However, no one group is more important than the other groups. We need them all, but in varying amounts.
3. Variety:
- Variety is important. No one-food group can provide all the nutrients we need.
4. Focus on Fat:
- Certain foods contain more than the recommended amounts of fats.
- They should be used sparingly.
In Basic Menu-planning for clients, consider the following:
- Client needs, limitations (special diet, soft foods)
- Client preferences -review likes/dislikes, favorite recipes
- Cost of food items
- Ease of preparation, re-serving, and re-heating.
- It is helpful at times to keep a log of client preference.
- Involve your client as much as possible in planning and preparing.
- Review cookbooks, magazines for ideas to present to your client.
Hints for Encouraging Improved Nutrition:
- As a caregiver, encourage proper nutrition. Gently share your knowledge. Recognize your client’s right to make his own decision.
- Be aware that very generous portions can overwhelm an elderly client. Elders do have decreased
- Need for caloric intake. Offer smaller portions of a variety of foods as possible.
- Encourage improved nutrition by updating your client on availability of appealing fresh produce.
- Brainstorm with your client on favorite recipes and foods.
- Read labels -educating yourself and your client.
- Be aware that many processed products contain “hidden” sugars and salt. By rinsing off
- Canned vegetables or fruit, you can remove some of the excess salt or sugar.
- Do not neglect the importance of fluid intake to your client’s health. Encourage your client to drink plenty of juice, milk, and water.
- Consider garnishes: They can add appeal to a meal while adding nutritional value.
Examples of Garnishes:
- Orange or pineapple slices, cut radish, slivers of green pepper, celery, carrots, cucumbers, tomato wedges.
Preparing the Meal Being aware of the amount of energy you use when preparing foods will save time, money, and your care recipient’s resources if you remember the following:
- Prepare one-dish meals.
- Make enough food for more than one meal and reheat the remaining servings.
- Use the correct burner size and correct pan size; a small pan should have a small burner.
- Do not preheat the oven more than necessary.
- When using the oven, prepare more than one item at a time.
- Turn off the heat on an electric range a few minutes before the food is ready.
- If possible, use a small toaster oven for small jobs and the big oven for bigger jobs. Other things to consider when preparing meals include:
- Wash your hands often during the preparations.
- When using spoons, etc. to taste foods, do NOT use them again without washing them first.
- Properly store any leftovers as soon as possible.
- Prepare leftovers in proper serving size.
- Thoroughly wash all fresh fruits and vegetables.
- Clean up as you go along and when you are done.
- Meats should be defrosted in fridge or microwave. Do NOT let them sit out at room temperature.
- Use as little water as possible when cooking vegetables.
- Remember to include fluids in the care recipient’s diet.
- Follow the menu and recipes.
- Know food substitutions allowed for a special diet if a food item is not available.
General Food Handling Hints
- Encourage clients not to overstock food that spoils easily.
- Keep refrigerators and freezer units in proper working condition.
- Refrigerator temperatures should be maintained at 36°F to 40°F.
- Freezer temperatures should be maintained at 0°F.
- Use foods by expiration date on package.
- Discard foods that show spoilage.
- Respect Client Rights. Explain the need to avoid use of spoiled food.
- Keep refrigerated foods properly covered or wrapped.
- Dry ingredients like flour, sugar, and pasta should be kept in covered containers.
- Foods purchased most recently should be used last.
- A rotation system should be used for canned goods.
- Foods in the refrigerator, as well as in dry storage, should have space around them for air circulation.
- Check dry storage areas periodically for signs of insects and rodent.
Fish, Poultry, and Other Meats:
- It is necessary to keep meats cold. Store them at 30 to 40 degrees F.
- Poultry, fish, and fresh meat such as roasts, chops, and steaks should be allowed some air.
- Loosen tight coverings. Cover the food and use it within a few days.
- Ground meat and variety meats, especially liver and brains, spoil more quickly than others.
- Store loosely wrapped. Cook within one or two days for best flavor or wrap in freezer paper and freeze.
- Cured and smoked meats, such as ham, frankfurters, bacon, and sausage (smoked and un-smoked)
- May be kept tightly wrapped while they are stored in the refrigerator. They keep longer than fresh
- Meals, although bacon and sausage are likely to change flavor.
- Keep cooked meat, poultry, fish, broth, and gravies covered and in the refrigerator. Use within a few days, or wrap well and freeze.
Storing leftovers:
Don’t cool leftovers on the kitchen counter. Put them straight into the refrigerator. Divide large portions of meat, macaroni, or potato salads, and large bowls of mashed potatoes or dressing into smaller portions. Small portions cool more quickly to temperatures at which bacteria quits growing.
Cleaning the Refrigerator
- Plan ahead. It can be time-consuming.
- Follow client instructions or posted instructions.
- Turn off the freezer. Note the original setting.
- Remove foods and place together in a bin or cooler to retain coldness.
- Some clients want food wrapped in towels or newspaper for further insulation.
- Place pan under drain inside refrigerator or turn up flip section of tray under freezer.
- Some clients request towels on the top-shelf inside refrigerator and on the floor in front of the refrigerator.
Defrosting the Refrigerator:
Several methods of defrosting include:
- Melt by steam from pans of boiling water placed inside freezer.
- Un-plug “Defrost Plug”(watch carefully!)
- Use hairdryer – avoid electrocution!
- Do not use a hairdryer with a wet hand or make direct contact with water.
- DO NOT use sharp instruments to pry loose ice buildup.
- Some appliances provide a blunt-ended, soft plastic tool (like a pancake turner) for gentle ice removal.
- Be patient. Ensure all ice has melted.
Wash Interior of Refrigerator and Replace Food
- Wipe interior of refrigerator with 3 tablespoons baking soda mixed in 1 quart of water.
- Turn on freezer unit when completed.
- Replace foods.
- Check for proper coldness setting.
Keep Hot Food Hot
- High food temperatures (165-212F) reached in boiling, baking, frying, and roasting kill most food poisoning bacteria. If you need to delay serving cooked food, you have to keep it at a holding temperature – roughly 140°F to 165°F.
- Steam tables and chafing dishes are designed to maintain holding temperatures.
- They don’t always keep food hot enough. So it’s not wise to
- Leave hot food out more than 2 hours.
- When cooked food is left out, unheated, the possibility of bacterial growth is of significant importance.
- Food temperatures drop quickly to room temperature where food poisons thrive.
- Follow these rules to serve hot foods safely – particularly meat and poultry that are highly susceptible to food po1sorung.
Cook thoroughly
- Cook meat and poultry to “doneness” temperatures. (Refer to cookbook).
- Make sure that meat and poultry are cooked all the way through.
- Use a meat thermometer. Insert the tip into the thickest part of the meat. Avoid fat or bone.
- For poultry, insert the tip into the thick part of the thigh next to the body.
Don’t interrupt cooking
- Cook meat and poultry completely at one time.
- Partial cooking may encourage bacterial growth before cooking is complete.
Cooking frozen food
- Allow frozen food more time to cook.
- Frozen foods require 1 ½ times the cooking time of non-frozen foods.
Thoroughly reheat leftovers
- Cover leftovers when reheating to retain moisture and guarantee that food will heat all the way through.
Bring gravies to a rolling boil before serving.
NEVER LEAVE FOOD OUT FOR MORE THAN TWO HOURS!
Keep Cold Food Cold
- The colder food is kept, the less chance bacteria will have to grow. That’s why food keeps so much longer in the freezer than in the refrigerator.
- To ensure the refrigerator and freezer are giving good protection against bacterial growth; check them with an appliance thermometer.
- The refrigerator should register 40°F (5° Celsius) or lower.
- The freezer should register 0°F.
Here are some tips for keeping meat, poultry, eggs, milk, cheese, and other perishable foods cold:
Refrigerating:
- Since repeated handling can introduce bacteria to meat and poultry, leave products in the store wrap unless the wrappers are torn.
- If torn, to prevent moisture loss, re-wrap meats in wax paper, plastic wrap, or aluminum foil.
Read the labels:
- Refrigerate canned meat – or poultry – or store it in a cool, dry place.
Freezing:
- Although “freezer burn” (white, dried-out patches on the surface of meat) won’t make you sick, it will cause meat to be tough and tasteless. To avoid freezer burn:
- Wrap meats in heavy freezer paper, plastic wrap, or aluminum foil.
- Place new items to rear of freezer,
- Move old items to front to ensure older items are used first.
- Write date on freezer packages to help you know which items should be used first.
Thawing:
The safest way to thaw meat and poultry is to take it out of the freezer and leave it in the refrigerator overnight. Normally, it will be ready to use the next day.
For faster thaw:
- Put the frozen package in a watertight plastic bag under cold water. Change the water often.
- The cold-water temperature slows bacteria that might grow in the outer, thawed portions of the meat while the inner areas are still thawing.
- If you have a microwave oven, you can safely thaw meat and poultry in it. Follow manufacturer’s directions.
Caution:
Do not thaw meat and poultry on kitchen counter.Bacteria multiply rapidly at room temperature.
-
Cooking with a Microwave. How to keep the kitchen safe.
Microwave Cooking Hints
Familiarize yourself with your client’s microwave. Read the Manual. First, try to boil a cup of water about 3 minutes on High. Microwaves (extra short radio waves) cook food by causing friction, or movement of molecules in the food. Outside edges tend to cook/heat up faster. Stirring of foods and rotation of containers can ensure more even heating.
General Guidelines:
- Microwave cooking is usually faster than stovetop or oven cooking. Microwaves use electromagnetic energy to excite moisture molecules in food and cause simultaneous heating throughout. Microwaves save energy over conventional cooking methods when cooking small or medium quantities of dense foods.
- Foods cooked in a microwave should be slightly undercooked and allowed to ‘stand’ while the heat equalizes and completes the cooking process.
- Microwave energy is absorbed by foods but reflected by METAL.
- Use glass, paper, plastic, china, pottery, or special microwave utensils.
- Do not use metal pans or aluminum foil in the microwave!
- Most microwaves are automatically set to cook at full power unless you select a different power level. (Defrost settings are 50% of full power).
- If uncertain about cooking times, select short cooking intervals and check the food frequently.
- Stir, turn and reposition food throughout the cooking time.
- Arrange foods with thickest parts toward outside of the oven, thinnest parts toward the center.
- Cover foods with glass, wax paper, or paper towel to prevent spattering and to cook foods more evenly. Remove the cover carefully to avoid being burned by the steam as it escapes.
- Foods with skins or membranes (potatoes, hot dogs, egg yolks) need to be pierced with a fork before cooking. They might explode as the steam builds inside them while cooking.
- Foods cooked in a microwave do not develop a “crust” or become “browned” as they would in a conventional oven with dry heat.
Reheating Cooked Foods:
Allow about 1 1/2 minutes of cooking time for each cup (8 Oz) of cooked food. When warming several different foods on the same plate, make sure the serving portions are similar for even heating.
Defrosting Frozen Foods:
Allow for ‘standing’ time between short cooking times. This allows the food temperature to equalize and avoids uneven cooking of the food. For each cup (8 Oz) of frozen, cooked food, microwave for one minute, and then let the food stand for 1 minute. Repeat until ice crystals have dissolved.
Foods That Microwave Well:
Vegetables, baked potatoes (first, pierce the skin with a fork) leftovers, scrambled eggs, fish, casseroles, puddings frozen entrees, and meatloaf.
How do I keep the kitchen safe?
Food preparation is a potentially dangerous job. Because of this, a high percentage of household injuries occur in kitchens. While preparing meals, people cut themselves with knives, with cans that food is packaged in, and with other objects and surfaces in the kitchen. They jab themselves with forks and bruise themselves by bumping into things. Such accidents occur even to experienced cooks. The key to avoiding these accidents is to be aware of the things that can hurt you. Think about what the possible results might be when you begin a task.
Things to be aware of for safety in the kitchen:
- Don’t cook grease at a high temperature
- Use potholders when handling hot pots and pans
- Clean up spills immediately
- Put utensils away where they belong
- Move about the kitchen with care
- Be careful when working with knives – take your time and watch what you are doing
- Wear appropriate clothing when cooking – no loose garments
- Do not use containers that are chipped or cracked.
-
General and therapeutic diets.

An individual’s diet is the sum of food and drink that he or she habitually consumes. Dieting is the practice of attempting to achieve or maintain a certain weight through diet. People’s dietary choices are often affected by a variety of factors, including ethical and religious beliefs, clinical need, or a desire to control weight.
Not all diets are considered healthy. Some people follow unhealthy diets through habit, rather than through a conscious choice to eat unhealthily. Terms applied to such eating habits include “junk food diet” and “Western diet”. Many diets are considered by clinicians to pose significant health risks and minimal long-term benefit. This is particularly true of “crash” or “fad” diets – short-term weight-loss plans that involve drastic changes to a person’s normal eating habits.
Types of Therapeutic Diets
A therapeutic diet is a meal plan that controls the intake of certain foods or nutrients. It is part of the treatment of a medical condition and are normally prescribed by a physician and planned by a dietician. A therapeutic diet is usually a modification of a regular diet. It is modified or tailored to fit the nutrition needs of a particular person.
Therapeutic diets are modified for (1) nutrients, (2) texture, and/or (3) food allergies or food intolerances.
Common reasons therapeutic diets may be ordered:
- To maintain nutritional status.
- To restore nutritional status.
- To correct nutritional status.
- To decrease calories for weight control.
- To provide extra calories for weight gain.
- To balance amounts of carbohydrates, fat and protein for control of diabetes.
- To provide a greater amount of a nutrient such as protein.
- To decrease the amount of a nutrient such as sodium.
- To exclude foods due to allergies or food intolerance.
- To provide texture modifications due to problems with chewing and/or swallowing
Common therapeutic diets include:
1. Nutrient modifications.
- No concentrated sweets diet;
- Diabetic diets;
- No added salt diet;
- Low sodium diet;
- Low fat diet and/or low cholesterol diet;
- High fiber diet;
- Renal diet.
2. Texture modification.
- Mechanical soft diet;
- Puree diet.
3. Food allergy or food intolerance modification.
- Food allergy;
- Food intolerance.
4. Tube feedings.
- Liquid tube feedings in place of meals;
- Liquid tube feedings in addition to meals.
5. Additional feedings – In addition to meal, extra nutrition may be ordered as:
- Supplements – usually ordered as liquid nutritional shakes once, twice or three times per day; given either with meals or between meals.
- Nourishments – ordered as a snack food or beverage items to be given between meals mid-morning and/or mid-afternoon.
- HS snack – ordered as a snack food or beverage items to be given at the hour of sleep.
6. The following list includes brief descriptions of common therapeutic diets:
Clear liquid diet –
- Includes minimum residue fluids that can be seen through.
- Examples are juices without pulp, broth, and Jell-O.
- Is often used as the first step to restarting oral feeding after surgery or an abdominal procedure.
- Can also be used for fluid and electrolyte replacement in people with severe diarrhea.
- Should not be used for an extended period as it does not provide enough calories and nutrients.
7. Full liquid diet.
- Includes fluids that are creamy.
- Some examples of food allowed are ice cream, pudding, thinned hot cereal, custard, strained cream soups, and juices with pulp.
- Used as the second step to restarting oral feeding once clear liquids are tolerated.
- Used for people who cannot tolerate a mechanical soft diet.
- Should not be used for extended periods.
No Concentrated Sweets (NCS) diet.
- Is considered a liberalized diet for diabetics when their weight and blood sugar levels are under control.
- It includes regular foods without the addition of sugar.
- Calories are not counted as in ADA calorie controlled diets.
Diabetic or calorie controlled diet (ADA).
- These diets control calories, carbohydrates, protein, and fat intake in balanced amounts to meet nutritional needs, control blood sugar levels, and control weight.
- Portion control is used at mealtimes as outlined in the ADA “Exchange List for Meal Planning.”
- Most commonly used calorie levels are: 1,200, 1,500, 1,800 and 2,000.
No Added Salt (NAS) diet.
- Is a regular diet with no salt packet on the tray.
- Food is seasoned as regular food.
Low Sodium (LS) diet.
- May also be called a 2 gram Sodium Diet.
- Limits salt and salty foods such as bacon, sausage, cured meats, canned soups, salty seasonings, pickled foods, salted crackers, etc.
- Is used for people who may be “holding water” (edema) or who have high blood pressure, heart disease, liver disease, or first stages of kidney disease.
Low fat/low cholesterol diet –
- Is used to reduce fat levels and/or treat medical conditions that interfere with how the body uses fat such as diseases of the liver, gallbladder, or pancreas.
- Limits fat to 50 grams or no more than 30% calories derived from fat.
- Is low in total fat and saturated fats and contains approximately 250-300 mg cholesterol.
High fiber diet.
- Is prescribed in the prevention or treatment of a number of gastrointestinal, cardiovascular, and metabolic diseases.
- Increased fiber should come from a variety of sources including fruits, legumes, vegetables, whole breads, and cereals.
Renal diet.
- Is for renal/kidney people.
- The diet plan is individualized depending on if the person is on dialysis.
- The diet restricts sodium, potassium, fluid, and protein specified levels.
- Lab work is followed closely.
Mechanically altered or soft diet.
- Is used when there are problems with chewing and swallowing.
- Changes the consistency of the regular diet to a softer texture.
- Includes chopped or ground meats as well as chopped or ground raw fruits and vegetables.
- Is for people with poor dental conditions, missing teeth, no teeth, or a condition known as dysphasia.
Pureed diet.
- Changes the regular diet by pureeing it to a smooth liquid consistency.
- Indicated for those with wired jaws extremely poor dentition in which chewing is inadequate.
- Often thinned down so it can pass through a straw.
- Is for people with chewing or swallowing difficulties or with the condition of dysphasia.
- Foods should be pureed separately.
- Avoid nuts, seeds, raw vegetables, and raw fruits.
- Is nutritionally adequate when offering all food groups.
Food allergy modification.
- Food allergies are due to an abnormal immune response to an otherwise harmless food.
- Foods implicated with allergies are strictly eliminated from the diet.
- Appropriate substitutions are made to ensure the meal is adequate.
- The most common food allergens are milk, egg, soy, wheat, peanuts, tree nuts, fish, and shellfish.
- A gluten free diet would include the elimination of wheat, rye, and barley. Replaced with potato, corn, and rice products.
Food intolerance modification.
- The most common food intolerance is intolerance to lactose (milk sugar) because of a decreased amount of an enzyme in the body.
- Other common types of food intolerance include adverse reactions to certain products added to food to enhance taste, color, or protect against bacterial growth.
- Common symptoms involving food intolerances are vomiting, diarrhea, abdominal pain, and headaches.
Tube feedings –
- Tube feedings are used for people who cannot take adequate food or fluids by mouth.
- All or parts of nutritional needs are met through tube feedings.
- Some people may receive food by mouth if they can swallow safely and are working to be weaned off the tube feeding.
Bland Diet
At times, due to gastro-intestinal or esophageal problems, clients need to follow a bland diet.
Ideas: Applesauce, toast, French to as cream of wheat or rice, oatmeal, simple muffins, cinnamon bread, pasta dishes such as macaroni and cheese, egg noodles with herbs or cheese, potatoes of all kinds – baked, mashed, scalloped, eggs: omelets, soft-boiled, egg salad, rice dishes, rice pudding, custards, puddings.
Special Diets:
If the physician recommends a special diet, the physician or nurse usually provides guidelines and sample menus.
-
Common Nutritional Problems and Helpful Suggestions.
Many clients prefer vegetables cooked soft, like canned, although some do enjoy today’s more popular steamed/crunchy style. The sense of smell can stimulate the appetite. Hot foods create aroma. Don’t easily accept “no” when a client says they aren’t hungry. Keep offering suggestions, and thinking of new creative ways to encourage nutrition.
The following are some helpful suggestions for Common Nutritional Problems:
- Nausea – Cold food is least apt to provide odor which often triggers nausea. Offer small portions, frequently. Eating slowly may be helpful.
- Depression – Client has lost interest in life and gives up eating.
- Pain – Serve food when pain relieving medication is most effective.
- Loneliness -Provide companionship at mealtime.
- Fatigue – Rest before meals may be beneficial.
- Small appetites -The client may need five or six small feedings of high quality foods. High protein and high calorie beverages may be easier to consume than large amounts of food.
- Decrease insenseoftasteandsmell – Serve meals that look, taste, and srnel1 good.
- Constipationmaylowerappetite – Correct by including fluids and fiber in diet.
- Chewing problems related to lack of teeth or poorly fitting dentures – Use tender cooked meats, ground meats like beef, lamb, fresh pork, ham, and veal. Serve meals of fish, eggs, cheese, and legumes. Use moist cooking methods or cook at low temperatures.
- Muscle control – Loss of muscle control may lead to changes in eating habits where. Clients avoid foods that may be difficult to cut or may be easily spilled.
- Improper mouth care – A bad taste in the mouth detracts from enjoyment of food.
- Economic situation – Living on a fixed or limited income limits food expenditures. Very often, less expensive foods are often selected which may be higher in carbohydrates and lower in protein.
- Transportation – Lack of adequate transportation may make shopping for bargains difficult and carrying bundles of groceries impossible.
- Social climate – Clients living alone may lack desire to prepare and eat regular meals. Snack foods may be used instead.
Everything the care recipient eats and drinks in a day should be included in the planning. This food may be eaten at the three regular meals and/or in the form of snacks during the day. It is important to plan meals as close as possible to the care recipient’s usual eating habits. When the care recipient’s diet is changed, take special care to try to keep this new diet as close to the diet of the other family members as possible. For example, when your client has a salt-free diet, separate this food from that of the other family members before salt is added. In other words, care recipients may have the same food as their family. They often will not keep to a prescribed diet, but will eat foods with which they are more familiar. In this case, encourage the care recipient to stay on a therapeutic diet.