Care for Individuals with Mobility Needs.
Limited Mobility, Bedrest
Effects of Limited mobility.
Limited Mobility Definition Mobility impairment may be caused by a number of factors, such as disease, an accident, or a congenital disorder and maybe the result from neuromuscular and orthopedic impairments. It may include conditions such as spinal cord injury, paralysis, muscular dystrophy, and cerebral palsy. It may be combined with other problems as well (i.e. brain injury, learning disability, hearing or visual impairment).
Symptoms Mobility impairment covers a wide range of impairment, from clients who can move quite freely with minimal assistance, to ones who rely on a motorized wheelchair. In some conditions, the person may experience pain, spasticity (continuous muscle contraction), or lack of coordination. In other conditions, there are intermittent flare-ups and periods of remission, where the client seems to have no impairment of function (i.e. multiple sclerosis). Some clients who use wheelchairs are able to stand, but not walk. Some may walk with the use of aid (canes, braces, and walker). The use of aid may increase fatigue.
- Complications of Bedrest.
Bed rest is a medical treatment in which a person lies in bed for most of some period of time to gain health benefits. Prolonged bed rest has long been known to have deleterious physiological effects, such as muscle atrophy and other forms of deconditioning such as arterial constriction. Besides lack of physical exercise, it was shown that another important factor is that the hydrostatic pressure (caused by gravity) acts anomalously, resulting in the altered distribution of body fluids. In other words, when getting up, this can cause an orthostatic hypertensive, potentially inducing a Vasovagal response. Even physical exercise in bed fails to address certain adverse effects.
It is also a major cause of thrombosis, mainly by reducing blood flow in the legs.
Tasks that may be performed by the personal care worker that prevent complications.
- Movement;
- Positioning;
- Alignment;
- Range of motion;
- Restorative care & rehabilitation.
Care for Individuals with Mobility Needs
Introduction:

It is important for direct care staff persons to follow infection control procedures to prevent illness. Of equal importance is taking steps to assist a client to be as mobile as possible. Mobility gives people the opportunity to socialize, be active and independent. If mobility becomes limited, a person’s opportunities shrink and choices are reduced. Serious complications can result from long periods of limited mobility.
While the thought of being less active may sound very soothing, it can lead to many complications that can cause problems in almost every major body system. Immobility can have the following effects:
- Difficulty breathing and in the ability to expand one’s lungs. This can result in fluid buildup in the lungs, which increases the risk of pneumonia and lung infections.
- The heart works harder to pump blood through a body laying flat. Possible problems with blood circulation are swelling, blood pooling in the legs decreases in blood pressure and increased risk of blood clots.
- Pressure sores develop quickly because the oxygen supply is reduced and pressure is increased.
- Muscles weaken and deteriorate from lack of use.
- Osteoporosis, fractures, slowed healing and other complications result because calcium is reduced in unexercised bones.
- If a person is in a flat position for a long time, urine does not fully drain out of the bladder and leftover urine in the bladder can become infected.
- There is a higher risk of choking and for developing indigestion or heartburn.
- A person’s appetite may decrease because they are less active or bored.
- Dehydration may become a problem as well.
- Mental health problems like depression become more common.
To help clients with mobility needs avoid these health risks, you can encourage them to be as active as possible, letting them do tasks, no matter how small, that they are able to do safely.
TURNING AND POSITIONING
Care recipients who are bedridden must have their position changed often. Learn how to give proper support and how to align the body properly in order to help them maintain or recover the best possible state of health. For instance, any open skin will heal more quickly if pressure is reduced and the air is allowed to circulate around it. The successful practice of body alignment means that all parts of the body are in their proper positions in relation to each other. For instance, the shoulders and the hips should be at the same height and angle. Care recipients can be positioned in many different ways, depending on their diagnosis, condition, and comfort. Remember that care recipients, might not stay in the correct position for a couple of hours even though they usually cannot move without help. Check their position often.
Some general guidelines of positioning include the following:
- Position and support only nonfunctional parts of the body, leaving the rest of the body to move freely so that blood can circulate. These may include shoulder blades, hips, hands, arms/elbows, or legs. Do NOT place anything under the knees when lying on the back.
- Any swollen limb should be kept higher than the heart where possible so that gravity will help the extra fluid drain from the limb.
- Use of assistive devices when positioning a client:
- Trochanter rolls;
- Footboards;
- Hand rolls;
- Bed cradles;
- Abdominal pillows;
- Abductor pillow;
- Pillows.
For example, a rolled-up washcloth makes an excellent support for the hand. Different sizes of pillows or pieces of foam can be used to support other parts of the body.
The different body positions used for positioning clients.
- Side-lying;
- Supine;
- Prone;
- Sim’s;
- High and low Fowler’s;
- Trendelenberg.
Sitting Up When care recipients are eating, watching television, visiting, reading, or if they have a heart or respiratory disorder, they will need to be positioned in bed sitting up. Good body alignment is very important. This involves keeping the spine straight and supporting the head with a small pillow. Place pillows elsewhere, such as under the hands, for further comfort. When care recipients do not have a hospital bed, raise them using an arm lock and then position pillows behind the back to the desired level.
Positioning on the Back Lying on the back is called the supine position. Align the care recipient’s body with the spine straight. Normally, all that is needed is a pillow under the head and, maybe, a rolled-up washcloth for the hands. Be sure to loosen the top sheet and blanket to relieve pressure from the toes. If the care recipient has nonfunctional body parts, more support will be needed. Nonfunctional means those parts of the body that cannot move due to paralysis from a stroke, resulting in a ‘weak’ side. This site requires more support and may include putting the following on that ‘weak’ side: 1. Small, folded hand towel under the shoulder blade. 2. Folded bath towel under the hip. 3. Rolled washcloth in the hand. 4. Arm and elbow on the pillow so they are higher than the heart. 5. A small pillow under the calf of the leg, with the heel hanging off the mattress edge. 6. Do NOT place anything under the knee.
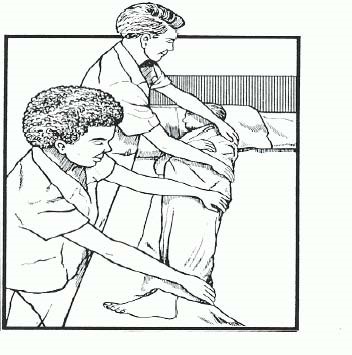
Turning
Sometimes, to prevent complications from bed rest and to receive care, bedridden care recipients must be turned. The direction in which they are moved will depend on the specific circumstances and conditions.
Procedure for Turning and Positioning
- Wash your hands.
- Explain to the care recipient what you are going to do.
- Provide privacy.
- Raise the bed to a comfortable working height.
- Lower the head of the bed as flat as possible.
- Raise the side rail on the opposite side from where you are working.
- Move the care recipient to the side of the bed near you.
- Cross the care recipient’s arms over the chest and nearest leg over the farthest leg.
- If turning away from you, stay on this side of the bed. If turning the care recipient toward you, move to the other side of the bed. Remember to pull the side rail up.
- Use good body mechanics with your feet separated, knees bent, and back straight.
- Place one of your hands on the care recipient’s shoulder and the other on the hip.
- Gently roll care recipient toward you OR push them away from you.
- Make sure the care recipient is in good alignment.
- Place pillows in appropriate areas for comfort and support:
- Against the back;
- Under head and shoulder;
- In front of the bottom leg;
- The top leg on a pillow in a flexed position;
- Under care recipient’s arm/hand
- Lower the bed.
- Wash your hands.
Turning techniques:

Draw sheet (lift sheet).
Log roll
To make turning and positioning a safe procedure for both you and your care recipient, remember the following basic rules:
- Always explain to the care recipient what you are going to do and why.
- Encourage the care recipient to help as much as possible.
- Always remember to lock the wheels on the bed.
- When safety rails are not provided on the bed, use common sense to provide safety measures during a procedure, such as moving the bed against a wall.
- If possible, raise the bed to a comfortable working height before performing a procedure and lower it when completed.
- Always provide privacy when performing a procedure.
- Use good body mechanics.
- Remember to protect any surgical tubing.
- Give the most support to the heaviest parts of the care recipient’s body. Usually, this is the trunk of the body, shoulders to hips.
- For the most support, hold the care recipient close to you when lifting.
- Move smoothly. Do not jerk.
- Tell your care recipient to move on the count of three when he/she is able to help you.
- The care recipient should be centered on the bed.
- Make sure the care recipient is comfortable before you leave. (Sitting Up when care recipients are eating, watching television, visiting, reading,)